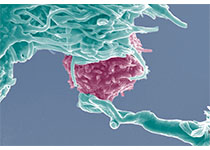
JAMA Oncology:原发肿瘤位置对III期结肠癌预后有影响吗?
2017-12-05 曹守波 肿瘤资讯
目前为止,尚未有数据支持原发肿瘤位置(primary tumor location, PTL)对结肠癌接受手术联合标准辅助化疗治疗患者预后的影响。最新一项研究对上述问题做了系统评价,研究发现,右侧部位肿瘤与转移性结肠癌较差的预后密切相关,RAS突变和/或BRAF突变的右侧部位肿瘤患者相比左侧有更好的无病生存期(disease-free survival, DFS)。而在RAS和BRAF基因均为野生
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#III#
26
#肿瘤位置#
46
#Oncology#
26
#原发肿瘤#
44
#Oncol#
35
学习并分享!!
68
学习了.谢谢分享!
63
学习了谢谢分享!!
62
#III期#
25
学习了.谢谢分享!
54