Spine:腰椎间盘突出症手术治疗远期疗效更佳
2014-01-14 佚名 丁香园
腰椎间盘突出症(LDH)是骨科常见病和多发病,是腰腿痛的常见病因之一。该病的治疗方法可分为手术与保守治疗两大类。为比较两种治疗方案的临床效果,由NIH资助,达特茅斯医学院脊柱外科杂志SPINE主编James Weinstein教授牵头,启动了一项SPORT试验(The Spine Patient Outcomes Research Trial)。【原文下载】 SPORT试验主要目的是比较保守治疗
腰椎间盘突出症(LDH)是骨科常见病和多发病,是腰腿痛的常见病因之一。该病的治疗方法可分为手术与保守治疗两大类。为比较两种治疗方案的临床效果,由NIH资助,达特茅斯医学院脊柱外科杂志SPINE主编James Weinstein教授牵头,启动了一项SPORT试验(The Spine Patient Outcomes Research Trial)。【原文下载】
SPORT试验主要目的是比较保守治疗与手术治疗对腰椎间盘突出症、腰椎管狭窄症以及退变性腰椎滑脱症三大腰椎退行性疾病及其所致腰腿痛的临床效果,以及两者之间成本效益比,是迄今为止美国NIH有关退变性腰腿痛疾病投入最大的临床研究,已发表数十篇文章,其中不乏NEJM,JAMA等顶级医学期刊。
近日,美国学者Jon D.Lurie等将SPORT试验中腰椎间盘突出症手术与保守治疗临床疗效对比研究成果发表在SPINE杂志上,该研究为一项前瞻性及观察性队列研究,患者随访时间超过8年。
经过严格的筛选,1244例符合纳入标准的腰椎间盘突出患者被招募参与此项研究,其中随机队列501例,观察队列743例,患者平均年龄41.7岁,无统计学差异。治疗方案包括标准椎间盘切除术(IDH)或者常规的保守治疗,最终治疗方案由患者及医生共同决定。
研究终点为6周、3月、6月以及每年直至8年。该研究主要疗效评估指标包括:SF-36躯体疼痛和生理机能(PF)评分表(0分最严重,100分最轻)和美国骨科协会MODEMS版Oswestry障碍指数(0分最轻,100分最重);次要疗效评估指标包括:坐骨神经痛SBI、症状改善情况、工作状况等。
研究结果显示:96%患者随访≥1年,63%的患者随访≥8年。在随机队列中,手术治疗组60%患者最终接受手术,保守治疗组48%患者最终接受手术治疗;在观察队列中,手术治疗组(521例),95%接受手术;保守治疗组(222例),56例(25%)选择保守治疗患者最终接受手术。
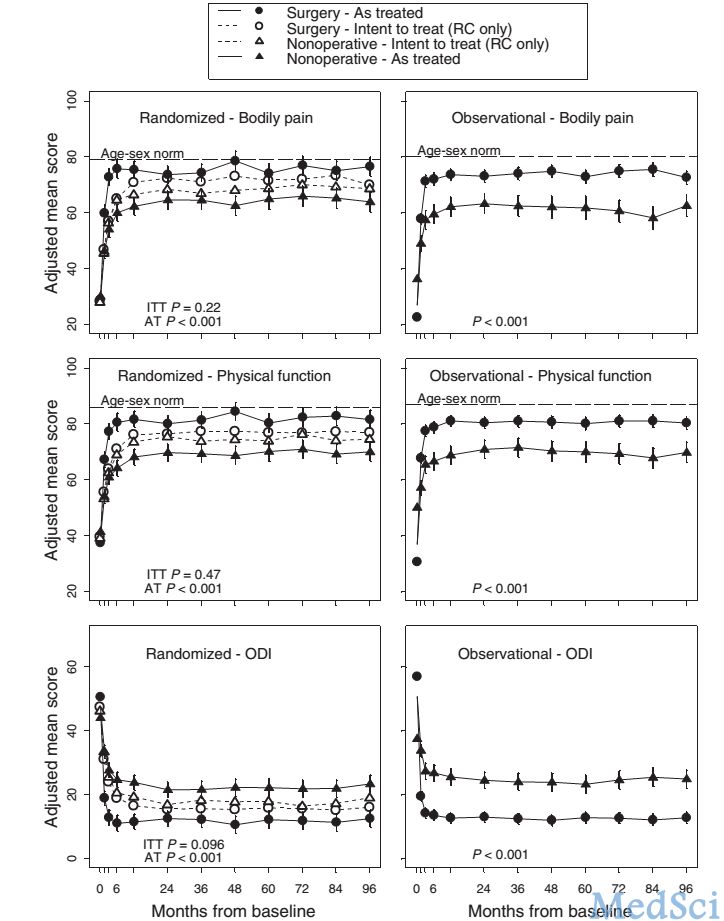
队列研究的ITT分析(intent-to-treat analysis)显示手术治疗可能更优,手术显著改善患者坐骨神经痛SBI,有统计学意义;但ODI、SF-36疼痛及PF改善无统计学意义。AT分析(as-treated analysis)显示手术治疗更佳,SF-36躯体疼痛评分、SF-36PF、ODI较保守治疗明显改善(如图1、图2)。
图 1:随机队列ITT分析示:SF-36躯体疼痛及PF、ODI无统计学差异。AT分析示:手术治疗主要评估指标优于保守治疗,SF-36躯体疼痛及PF、ODI有统计学差异
图 2:随机队列ITT分析及AT分析均示:手术治疗次要评估指标优于保守治疗且有统计学意义
因患者组间交叉数量较多,对结果进行意向性治疗分析(ITT)发现,术后8年,手术组患者较保守治疗组患者在主要临床功能指标上无显著差异,但次要指标如坐骨神经痛,自我症状改善等手术组显著好于保守治疗组;接受治疗分析(as to treat analysis)结果显示,手术组患者主要功能指标均显著好于保守治疗组;手术或保守治疗患者8年后功能均得到显著改善,改善效果持续存在。
作者认为对严格把握手术指征的患者,手术治疗可以获得较保守治疗更多的收益;术后8年时间内手术治疗症状改善效果持续存在。
原文出处:
Lurie JD, Tosteson TD, Tosteson AN, Zhao W, Morgan TS, Abdu WA, Herkowitz H, Weinstein JN.Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial.Spine (Phila Pa 1976). 2014 Jan 1;39(1):3-16. doi: 10.1097/BRS.0000000000000088.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#椎间盘突出#
34
#Spine#
27
#远期疗效#
33
#腰椎#
34
#手术治疗#
33
#腰椎间盘#
24