Anal. Chem:微生物所在微滴数字PCR技术研制方面取得进展
2019-01-08 MedSci 微生物研究所
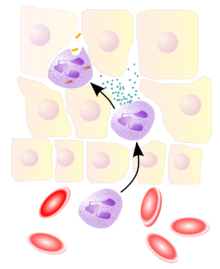
数字PCR是一种用于绝对核酸定量检测方法,具有前所未有的准确度和精确度,是继实时荧光定量PCR技术之后的第三代核酸定量扩增检测技术,在液体活检、肿瘤伴随诊断、无创产前筛查、病原载量监测等方面具有重要应用前景,是科研和临床领域的平台级新技术。数字PCR市场主流产品主要为欧美跨国公司的高端仪器,在科研和临床的应用还比较初步。数字PCR的更广泛使用和临床应用,仍然存在几个主要挑战,包括降低成本,集成仪器
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ANA#
26
学习了谢谢分享
41
#微生物#
25
学习了谢谢分享
50
#Anal#
37
#PCR#
34
学习了,谢谢分享
41