Antiviral Res:王建华等III型干扰素IFNλ抗HIV-1研究获进展
2012-05-24 上海巴斯德研究所 上海巴斯德研究所
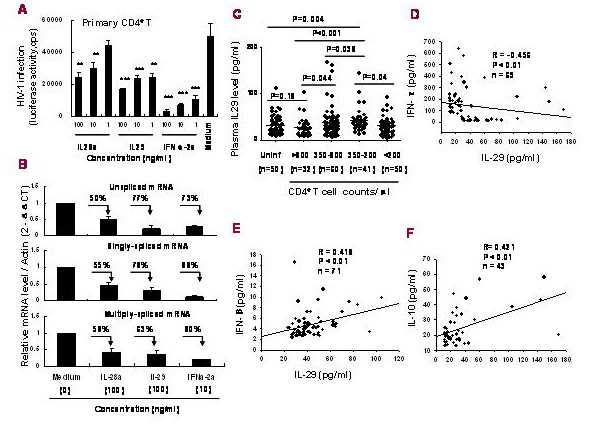
图 A) IFNλ抑制HIV-1在T细胞内的复制;B)HIV-1基因转录后剪切产物的定量;C)HIV-1感染者血浆IL-29水平随着外周血CD4+ T细胞的下降而升高;D,E和F) HIV-1感染者血浆IL-29分泌与细胞因子的相关性分析。 2012年5月,国际著名学术期刊Antiviral Research在线发表了中国科学院上海巴斯德研究所王建华研究组关于IFNλ抗HIV-1感染最新研究成果

图 A) IFNλ抑制HIV-1在T细胞内的复制;B)HIV-1基因转录后剪切产物的定量;C)HIV-1感染者血浆IL-29水平随着外周血CD4+ T细胞的下降而升高;D,E和F) HIV-1感染者血浆IL-29分泌与细胞因子的相关性分析。
2012年5月,国际著名学术期刊Antiviral Research在线发表了中国科学院上海巴斯德研究所王建华研究组关于IFNλ抗HIV-1感染最新研究成果。
病毒感染能够诱导干扰素的产生。依据细胞表面干扰素受体的特征,可将干扰素分为I、II及III型干扰素。III型干扰素(interferon lambda,IFNλ)是一类新型干扰素,包括三个家族成员:IL28a (IFNλ2)、IL28b(IFNλ3)及IL29 (IFNλ1),它们具有类似的组成和结构。已有的报道表明,IFNλ如同干扰素家族的其它成员一样,也具有抑制HCV、HBV等病毒复制的功能。然而,IFNλ在抗HIV研究方面的报道甚少。
上海巴斯德所病毒免疫学研究组田仁荣及其合作者在组长王建华研究员的指导下,深入分析了IFNλ对HIV-1复制的抑制作用及机制。研究发现,IL28a 和IL29能够通过诱导抗病毒基因MxA、OAS及PKR的表达,而抑制HIV-1在人基因组的整合及抑制病毒基因转录后的剪切等环节;临床数据分析显示,病人血浆中IL29的水平与外周血中CD4+ T细胞数呈负相关,与病毒载量并非显示为负相关;在细胞因子分泌方面,血浆中IL29的水平与IFNβ以及IL10呈正相关,而与IFNγ呈负相关,提示IL29可能参与了机体抗HIV-1免疫反应的调节。
这一结果加深了人们对III型干扰素在HIV-1感染中所发挥作用的理解,有助于进一步揭示机体抗病毒反应机制与寻找新的抗病毒策略。
该项研究是与江苏省疾病预防与控制中心、南京医科大学第一附属医院合作完成的,得到了中科院、国家自然科学基金委及上海市等的项目资助。(生物谷Bioon.com)

PMC:
PMID:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#研究获进展#
28
#Antiviral#
35
#III#
22
#I型干扰素#
27
#IFN#
25