Nat commun:在ccRCC中,HIF可通过脂肪酸代谢抑制促使脂质沉淀和癌变
2017-12-09 AlexYang MedSci原创
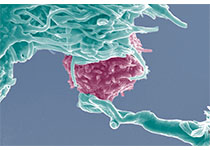
透明细胞肾细胞癌(ccRCC)是通过它的脂质和糖原在细胞质中沉积的组织学特点来鉴定的。VHL肿瘤抑制子的改变稳定化缺氧诱导因子(HIFs)是透明细胞肿瘤中最为常见的分子特性。但是脂质沉积的意义仍旧未被鉴定。最近,有研究人员通过鉴定线粒体脂肪酸转运、HIF直接靶标基因-棕榈酰基转移酶1A(CPT1A)的限速组分描述了脂质沉积的机制。研究发现,CPT1A可以由HIF1和HIF2抑制,减少脂肪酸转运到线
透明细胞肾细胞癌(ccRCC)是通过它的脂质和糖原在细胞质中沉积的组织学特点来鉴定的。VHL肿瘤抑制子的改变稳定化缺氧诱导因子(HIFs)是透明细胞肿瘤中最为常见的分子特性。但是脂质沉积的意义仍旧未被鉴定。最近,有研究人员通过鉴定线粒体脂肪酸转运、HIF直接靶标基因-棕榈酰基转移酶1A(CPT1A)的限速组分描述了脂质沉积的机制。研究发现,CPT1A可以由HIF1和HIF2抑制,减少脂肪酸转运到线粒体中,并且可促使脂肪酸转化为脂质滴来储存。研究发现,脂质滴的形成与脂质源无关,只在CPT1A受抑制时产生。因此,从功能上讲,CPT1A的抑制对肿瘤的形成非常关键,并且CPT1A表达的提高可以限制肿瘤的生长。在人类肿瘤中,CPT1A的表达和活性和正常肾脏比较降低,并且不良病人治疗结果与CPT1A在TCGA肿瘤中更低的表达有关。最后,研究人员指出,他们的研究鉴定了HIF对脂肪酸代谢的控制,并可以作为ccRCC肿瘤形成过程的必要成员。原始出处:Weinan Du, Luchang Zhang, Adina Brett-Morris et al. HIF drives lipid depositio
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
24
#CRC#
25
#RCC#
34
#Nat#
26
学习了.涨知识
52
#HIF#
40
#癌变#
37