J INTERN MED:人工瓣膜心内膜炎的微生物病因学分析
2022-04-07 MedSci原创 MedSci原创
在世界范围内,人工心脏瓣膜在瓣膜性心脏病患者中的应用越来越多。在主动脉瓣疾病中,较年轻的患者通常采用机械心脏瓣膜,而较年长的患者通常采用生物或经导管主动脉瓣置入术(TAVI)。人工瓣膜心内膜炎(PVE
在世界范围内,人工心脏瓣膜在瓣膜性心脏病患者中的应用越来越多。在主动脉瓣疾病中,较年轻的患者通常采用机械心脏瓣膜,而较年长的患者通常采用生物或经导管主动脉瓣置入术(TAVI)。人工瓣膜心内膜炎(PVE)是心脏瓣膜手术后的并发症。对不同类型PVE的细菌学差异的研究十分有限。
近日,内科学领域权威杂志Journal of Internal Medicine上发表一篇研究文章,该研究的目的是探讨PVE的微生物学与人工瓣膜类型和诊断时机之间的关系。
这项基于瑞典登记的以PVE为重点的感染性心内膜炎的回顾性研究,队列被分为机械瓣膜和生物瓣膜,心内膜炎定位于主动脉瓣、二尖瓣或三尖瓣,以及早期和晚期PVE。研究人员对这些组的微生物学进行了比较,此外,研究人员采用多变量logistic回归分析了金黄色葡萄球菌致PVE的预测因子。
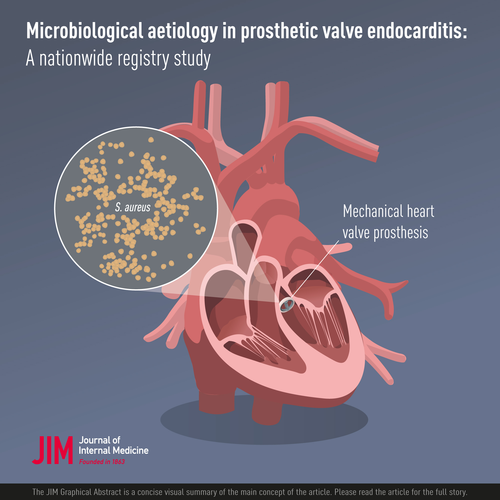
研究人员对749例患者780次PVE的致病微生物分布情况进行了比较。最常见的病原体包括-溶血性链球菌(29%)、金黄色葡萄球菌(22%)、肠球菌(14%)、凝固酶阴性葡萄球菌(CoNS)(12%)和痤疮皮杆菌(6%)。与生物瓣膜相比,机械瓣膜上更容易出现金黄色葡萄球菌(36% vs. 17%, p<0.001),而α-溶血性链球菌、肠球菌和con在生物瓣膜上更常见。在影响二尖瓣或主动脉瓣的PVE患者中,早期和晚期PVE患者的微生物学差异无统计学意义。由金黄色葡萄球菌引起的PVE预测因素有终末期肾病、静脉用药、机械瓣膜和三尖瓣心内膜炎。
由此可见,人工心脏瓣膜的类型与致病菌有关。机械瓣膜患者更易发生金黄色葡萄球菌引起的PVE。
原始出处:
Blerand Berisha,et al.Microbiological aetiology in prosthetic valve endocarditis: A nationwide registry study.Journal of Internal Medicine.2022.https://onlinelibrary.wiley.com/doi/10.1111/joim.13491
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内膜#
50
#微生物#
36
#人工瓣膜#
53
#心内膜炎#
47
#瓣膜#
42
#Med#
33