Chest:淋巴结受累范围或可预测非小细胞肺癌患者的预后
2013-12-27 佚名 丁香园
研究要点: 1)该研究评估淋巴结受累范围和其他预后因素在预测中国Ⅱ-N1期非小细胞肺癌患者确定性手术后结局中的意义; 2)发现肿瘤体积和淋巴结受累范围是整体生存期和无病生存期的重要预测因子。 在2009年发布的第7版国际抗癌联盟和美国癌症联合委员会癌症分期手册中,非小细胞肺癌(NSCLC)分期系统对当前的NSCLC淋巴结转移描述没有做任何修改。然而,NSC
研究要点:
1)该研究评估淋巴结受累范围和其他预后因素在预测中国Ⅱ-N1期非小细胞肺癌患者确定性手术后结局中的意义;
2)发现肿瘤体积和淋巴结受累范围是整体生存期和无病生存期的重要预测因子。
在2009年发布的第7版国际抗癌联盟和美国癌症联合委员会癌症分期手册中,非小细胞肺癌(NSCLC)分期系统对当前的NSCLC淋巴结转移描述没有做任何修改。然而,NSCLC患者淋巴结受累范围(包括受累淋巴结区、受累淋巴结比例和数目)的预后意义尚不清楚。
为了评估淋巴结受累范围和其他因素对确定性手术后的中国Ⅱ-N1期NSCLC患者预后的意义,来自上海交通大学附属上海市胸科医院的陆舜教授及其团队进行了一项研究,研究结果发表在2013年10月的Chest杂志上。研究发现,N1淋巴结转移、受累淋巴结比例和肿瘤大小可以为Ⅱ期NSCLC患者提供独立的预后信息。
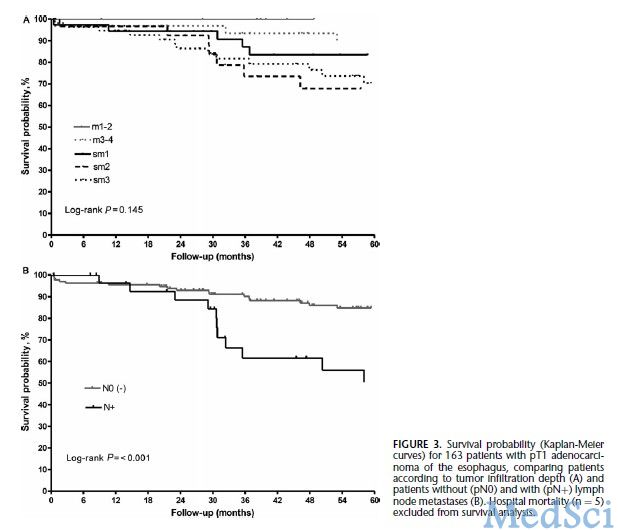
该研究回顾性分析了1999年至2009年期间,在上海市胸科医院进行完全手术切除的206例Ⅱ期(T1a-T2bN1M0)NSCLC患者的临床病理特征。使用Kaplan-Meier统计分析比较整体生存期(OS)和无病生存期(DFS)。使用分层回归分析和Cox回归分析评估淋巴结受累与生存期之间的关系。
该研究结果表明,单因素分析显示,外周淋巴结受累、受累淋巴结比例、肿瘤体积小和鳞状细胞癌可作为有统计学意义的指标预测较长的整体生存期和无病生存期。单因素分析同样证实脏层胸膜受累也可以作为一个有统计学意义的指标预测无病生存期。多因素分析显示肿瘤体积和淋巴结受累区域是整体生存期的重要预测因子。
该研究提示, N1淋巴结转移、受累淋巴结比例和肿瘤大小可以为Ⅱ期非小细胞肺癌患者提供独立的预后信息。
研究背景:
肺癌是世界范围内癌症相关死亡的主要原因。手术切除癌症组织是早期非小细胞肺癌的标准治疗方法。准确的淋巴结受累分期在小细胞肺癌患者起始治疗中是至关重要的。这经常影响治疗方法和治疗时机的决策。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
28
#Chest#
33
#肺癌患者#
29
#非小细胞#
19
#淋巴结#
27
#非小细胞肺癌患者#
35