NEJM:心脏支架术后采用双抗治疗,30个月优于12个月?(DAPT研究)
2014-11-19 睿智 MedSci原创
放支架了,也就是冠状动脉支架治疗缺血性心脏病,每年全世界可能有数以百万计的患者接受这样的治疗。关于术后,尤其是一年以后该如何治疗,近些年一直是学术界及心内科医生争论的众矢之的。新英格兰杂志11月16日新鲜出炉了最权威的研究! 虽然药物洗脱支架与裸金属支架相比,减少再狭窄率, 但人们仍然担心, 治疗一年后,药物洗脱支架可能引发支架血栓。支架血栓形成并不常见,但它常与心肌
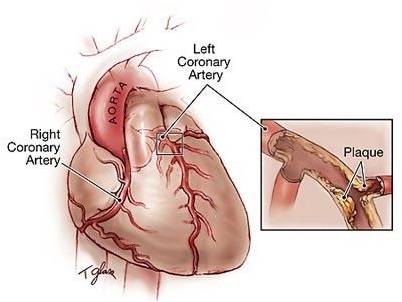
虽然药物洗脱支架与裸金属支架相比,减少再狭窄率, 但人们仍然担心, 治疗一年后,药物洗脱支架可能引发支架血栓。支架血栓形成并不常见,但它常与心肌梗死相伴,带来致命威胁。此外, 缺血性事件, 如心肌梗塞、中风、或心血管相关致死性事件,与治疗无关的冠状动脉病变,也可能在放入 支架后1年出现。
使用双重抗血小板治疗的P2Y12-receptor抑制剂结合阿司匹林,对预防冠状动脉支架血栓形成是至关重要的。这种疗法是目前推荐的药物洗脱支架植入后6到12个月的治疗方法。虽然一些观察性研究表明,在术后超过1年仍坚持双重抗血小板治疗,与降低心肌梗塞的风险相关,几个试验显示这样出血的风险会增加,且不能减少心肌梗死的发生率。是否应该继续双重抗血小板治疗,用以降低心血管支架未来血栓形成或缺血性事件发生,尚未以随机试验的方法确定。
DAPT研究,是多国多中心、随机、安慰剂对照试验, 旨在确定在接受一个冠状动脉支架治疗后超过一年,仍然继续双重抗血小板治疗的益处和风险。
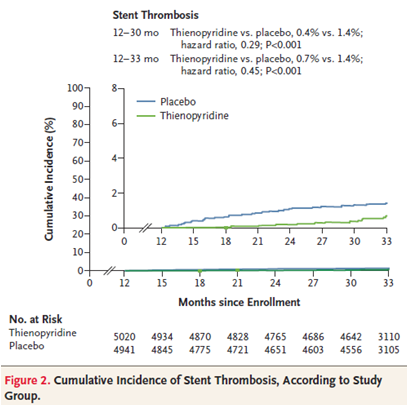
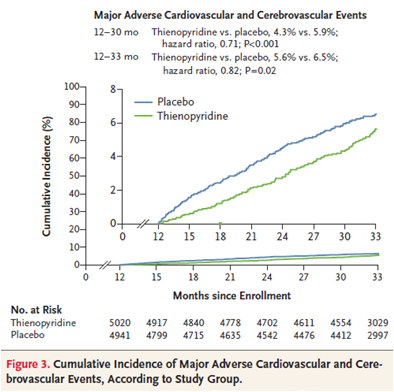
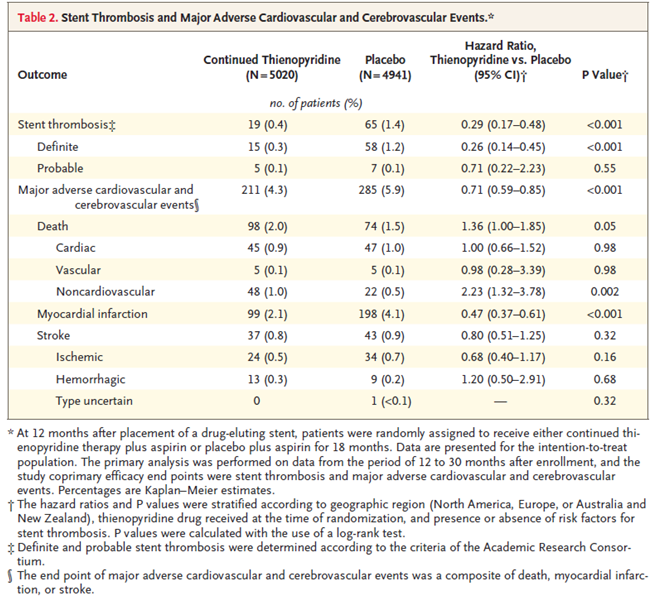
9961名患者被随机分配,一组在支架术后一年后继续thienopyridine治疗,另一组接受安慰剂治疗。与安慰剂组相比,thienopyridine继续治疗组减少了支架血栓形成率 (0.4%比1.4%; 危险比0.29,95% CI 0.17-0.48 ,P < 0.001) ,减少了主要不良心血管和脑血管事件(4.3%比5.9%; 危险比0.71, 95% CI, 0.59-0.85 ,P < 0.001)。与安慰剂组比较,thienopyridine治疗的心肌梗死率较低 (2.1%比4.1%; 危险比0.47; P < 0.001)。 全因死亡率thienopyridine治疗组是2.0%,安慰剂组是1.5% (风险比1.36,95% CI, 1.00 - 1.85; P = 0.05)。thienopyridine治疗中度或重度出血增加(2.5%比1.6%,P = 0.001)。
这一研究的意义在于,是第一个RCT研究,向人们证实了术后坚持双联抗血小板治疗的利大于弊,而RCT研究仍然是目前为止被认为最有说服力的科学实验。
我国虽为患者大国,这样的RCT试验却并不常见,更不要说包括9000余名患者在内, 基于本土数据的研究对我国的临床应用势必意义非凡。
MedSci原创征稿,未经授权不得以任何形式转载,谢谢!
原始出处:
Laura Mauri, M.D., Dean J. Kereiakes, M.D., Robert W. Yeh, M.D., Priscilla Driscoll-Shempp, M.B.A., Donald E. Cutlip, M.D., P. Gabriel Steg, M.D., Sharon-Lise T. Normand, Ph.D., Eugene Braunwald, M.D., Stephen D. Wiviott, M.D., David J. Cohen, M.D., David R. Holmes, Jr., M.D., Mitchell W. Krucoff, M.D., James Hermiller, M.D., Harold L. Dauerman, M.D., Daniel I. Simon, M.D., David E. Kandzari, M.D., Kirk N. Garratt, M.D., David P. Lee, M.D., Thomas K. Pow, M.D., Peter Ver Lee, M.D., Michael J. Rinaldi, M.D., and Joseph M. Massaro, Ph.D. for the DAPT Study Investigators.Twelve or 30 Months of Dual Antiplatelet Therapy after Drug-Eluting Stents.November 16, 2014DOI: 10.1056/NEJMoa1409312
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#支架术#
36
#支架术后#
33
非常好的文章,为PCI术后抗凝时间长度选择提供了依据。
112
#DAPT#
45
#双抗治疗#
47
#心脏支架#
41
#双抗#
31
心梗发病太多,术后一二级预防很重要啊!
110
非常好的文章
107
很有价值
115