-
利尿剂
-
血管紧张素转换酶抑制剂(ACEI)
-
血管紧张素受体拮抗剂(ARB)
-
沙库巴曲缬沙坦
-
β受体阻滞剂
-
螺内酯
-
伊伐布雷定
-
使用利尿剂要使患者达到“干重”状态;
-
RAS抑制剂和β受体阻滞剂应达到目标剂量或耐受剂量;
-
螺内酯国内推荐的最大剂量为每天20 mg(起始剂量从10 mg/d开始);
-
伊伐布雷定目标剂量为7.5 mg bid(起始剂量从2.5 mg bid开始)。
-
一是应用RAS抑制剂和β受体阻滞剂阻断过度激活的神经内分泌系统;
-
二是应用利尿剂消除液体潴留(适当的容量负荷管理);
-
三是β受体阻滞剂和伊伐布雷定联合使用使心率在静息状态下达到55~65次/分(优化的心率管理)。
-
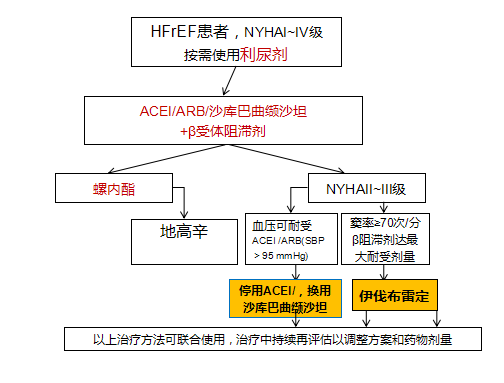
第一步,如患者存在液体潴留,应使用利尿剂,目前80%左右的患者都应使用利尿剂治疗;
-
第二步,加入RAS抑制剂及β受体阻滞剂形成治疗的“黄金搭档”;
-
第三步,加入螺内酯形成治疗“金三角”;
-
第四步,窦性心律患者心率增快在70次/分以上,可加用伊伐布雷定。仍有症状患者也可以加用地高辛;
-
第五步,如在第二步中使用的是ACEI或ARB,此时可以用沙库巴曲缬沙坦替换ACEI或ARB。需要指出的是,近几年的一系列研究提示,该药和ACEI/ARB一样,也可以用于尚不稳定的心衰患者如出院前和出院后的早期患者,即在心衰的全程应用,且由于该药在许多方面占优,故亦可作为RAS抑制剂起始选用的药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#金三角#
66
学习了
59
感谢老师分享
71
学习了
73
很好,学习了
61