JCO:HPV相关口咽癌的生物标志物被发现
2013-06-19 Alex 译 医学论坛网
研究人员发现,人类乳头状瘤病毒抗体也许可以鉴别出哪些人患HPV-相关口咽癌的风险大大增加,口咽就是喉咙的一部分,包含扁桃体。 在他们的研究中,至少三分之一的口咽癌患者体内存在HPV抗体,而没有患癌症的人中少于一百分之一。目前,这些抗体可以在发病前很多年检测到。也许有一天验血可以用来鉴别这种癌症,这些发现提高了这种可能性。 这

研究人员发现,人类乳头状瘤病毒抗体也许可以鉴别出哪些人患HPV-相关口咽癌的风险大大增加,口咽就是喉咙的一部分,包含扁桃体。
在他们的研究中,至少三分之一的口咽癌患者体内存在HPV抗体,而没有患癌症的人中少于一百分之一。目前,这些抗体可以在发病前很多年检测到。也许有一天验血可以用来鉴别这种癌症,这些发现提高了这种可能性。
这项研究是由美国国家癌症研究所(NCI)的科学家开展的,与国际癌症研究机构(IARC)合作,结果发表在2013.6.17 Journal of Clinical Oncology.
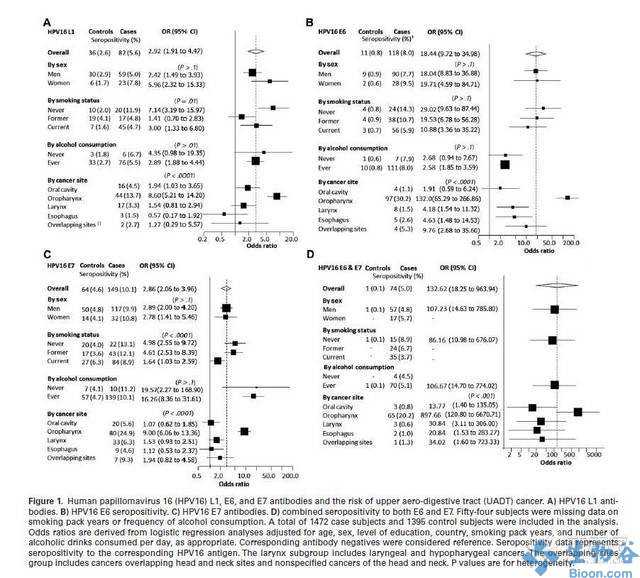
以前的观点认为,多数口咽癌可能与吸烟和饮酒有关,而不是HPV感染。然而,恶性肿瘤在世界的许多地方发生率都在增加,尤其是在美国和欧洲,因为感染人乳头状瘤病毒-16(HPV 16)的人在增加。在美国,据估计目前60%以上口咽癌患者是由于与HPV16感染有关。HPV16持续感染导致细胞发生变化,最终导致癌症。
HPV E6是有助于肿瘤的形成的病毒基因。关于HPV相关口咽癌的以往研究发现,患者血液中存在E6抗体。
“我们的研究不仅表明E6抗体可以在诊断前被检测到,在其许多情况下,一些抗体也可以在临床癌症诊断前超过十年可以检测到,这是筛选生物标志物的一个重要特征。”Aimee R. Kreimer博士说,他是NCI癌症流行病学和遗传学部的首席研究员。
Kreimer和她的同事检测了参加人员的样品,他们参与了欧洲前瞻性癌症与营养研究,这是一项来自10个欧洲国家的超过500,000名健康人的长期研究。研究开始时抽取参与者的血液试样,因为它们的初始的贡献,之后一直跟踪研究。
研究人员分析了135个在一年到13年间患有口咽癌的患者血液,也分析了1600个没有患上癌症的对照者血液。研究发现在35%癌症患者中可以检测到HPV16 E6蛋白抗体,而无癌症患者中检测率小于1%。血样平均在诊断前6年收集的,但血样收集和诊断之间的时间关系是独立的。HPV16 E6蛋白抗体甚至可以在诊断前10年在血液中发现。
科学家指出,HPV16 E6抗体或成为提升生存几率的生物指标,这与之前所报导的研究结果一致。研究显示,与HPV16 E6 抗体检测呈阴性的口咽癌患者相比,在整个随访过程中,确诊口咽癌前HPV16 E6抗体检测结果阳性的患者生存率要高70%。
国际癌症研究机构(IARC)的首席研究员Paul Brennan博士说:“尽管看似很有前景,但这些发现仍应被看作只是初步的断定。如果在其他的研究中HPV16 E6抗体的作用仍能保持这种体现,我们或可考虑为其建立一个筛查工具。
Scientists find promising biomarker for predicting HPV-related oropharynx cancer
Researchers have found that antibodies against the human papillomavirus (HPV) may help identify individuals who are at greatly increased risk of HPV-related cancer of the oropharynx, which is a portion of the throat that contains the tonsils....
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#标志物#
32
#JCO#
24
#口咽癌#
34
#生物标志#
0
#生物标志#
33