“靶环征”在产前超声诊断肛门闭锁中的意义
2018-08-23 袁鹰 李胜利 文华轩 中华超声影像学杂志
肛门闭锁(imperforate anus)由后肠发育缺陷或迟缓引起,是一种较常见的先天性畸形,发病率约占活产儿的0.02%~o.08%。该病可与其他先天性畸形或染色体异常,诸如21一三体、DiGeorge综合征、VACTERL联合畸形相伴随,因此对其进行产前筛查具有重要的临床指导意义。

肛门闭锁(imperforate anus)由后肠发育缺陷或迟缓引起,是一种较常见的先天性畸形,发病率约占活产儿的0.02%~o.08%。该病可与其他先天性畸形或染色体异常,诸如21一三体、DiGeorge综合征、VACTERL联合畸形相伴随,因此对其进行产前筛查具有重要的临床指导意义。
然而产前超声诊断肛门闭锁较困难,缺乏特征性表现,主要依赖于一些间接的超声表现,如闭锁肠管近段扩张、肠管内胎粪钙化或肠石症等。新近资料显示通过观察胎儿肛门括约肌声像图来诊断胎儿肛门闭锁,这有可能成为产前超声筛查肛门闭锁的一种新方法,但相关报道甚少,尤其缺乏大样本的临床数据。
本研究试图通过较大样本量的正常与异常胎儿肛门的超声图像特征,评估子宫内胎儿肛门括约肌发育并判断“靶环征”的诊断价值,以期为肛门闭锁的产前筛查提供新的理论依据。
资料与方法
一、研究对象
异常组:收集2003年1- 12月在我院行产前超声检查、产后新生儿检查或尸检证实为肛门闭锁胎儿48例,其中包括合并直肠泌尿道瘘或阴道瘘24例,该24例均伴有直肠扩张或阴道扩张;另有合并其他系统畸形且不伴瘘的肛门闭锁24例,未见直肠或阴道扩张。孕妇年龄20~36岁,平均(27.9±3.9)岁,行产前超声检查时胎儿孕周17~40周,平均(29.2±6.2)周。
正常对照组:选取2013年1-6月间孕18~41周单胎813例,入选标准:无母体疾病,既往无不良妊娠史,月经规则,实验室检查包括AFP、PAPPA、p-HCG无异常,胎儿系统超声检查无阳性发现,生后排便正常。按不同孕周又分为24个亚组。孕母年龄18~43岁,平均(29.1±4.4)岁。
二、仪器与方法
正常胎儿组为在我院常规行工、Ⅱ、Ⅲ级产前超声筛查者,对胎儿肛门进行横切面检查。在获取胎儿膀胱横切面后声束平面逐渐向胎儿尾侧方向平行移动,在臀部皮肤消失前两侧臀部之间可显示“高一中一高”同心圆样回声,此即为胎儿肛门横切面图像,称之为“靶环征”,在此切面上测量其直径、周长和面积。直径为“靶环征”的左右径,测量外周高回声线左右边缘之间的距离。采用电子轨迹球沿外周高回声边缘测量其周长与面积。每例测量3次,取其平均值。
对于肛门闭锁胎儿,不能显示“靶环征”者,上述测值以0计算。
由2名从事产前超声诊断工作5年以上的超声医师独立分析,分别给出诊断意见,对于有争议的病例交上级医师会诊,最后得出统一的结论。
结果
一、肛门括约肌声像图表现
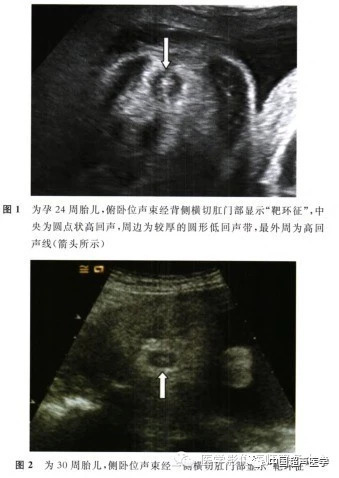
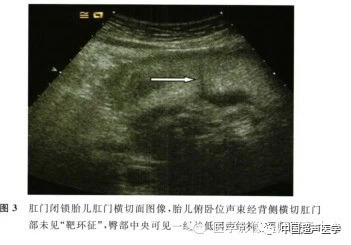
正常胎儿肛门括约肌在横切面图上表现为“靶环征”,即胎儿会阴部横切面中央显示为一同心圆形结构,中央为圆点状高回声,周边为较厚的圆形低回声带,最外周为圆形高回声线(图1,2)。
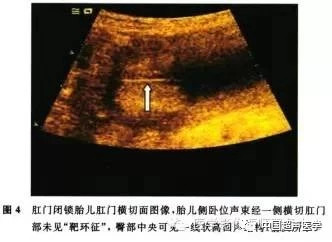
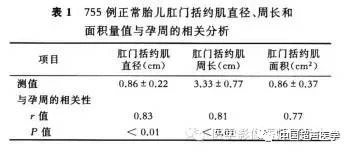
肛门闭锁胎儿肛门横切面上不能显示“靶环征”声像,代之为一直线状回声,当声束平面从胎儿背侧(图3)或腹侧入射时,表现为低回声线,当声束平面从胎儿左侧(图4)或右侧入射时,表现为高回声线。
二、“靶环征”显示率
正常组813例胎儿,其中755例可见“靶环征”,58例显示不清,显示率为92.7%(755/813)。随着孕周时间的延长,“靶环征”显示率逐渐增加。在胎龄21~37周,显示率最佳,稳定在97%~100%之间。不能显示“靶环征”的58例正常胎儿,也不能显示肛门部的现状低回声或高回声,肛门部横切面因为胎儿体位的关系不能显示出这一切面。所有异常组肛门闭锁胎儿均不能显示“靶环征”,而表现为低回声或高回声线。
三、胎儿肛门括约肌的官内发育
相关分析显示随着孕周的增长,755例正常组胎儿肛门直径、周长和面积均呈线性增加(表1)。通过回归分析得出各测值与孕周的直线回归方程式:肛门括约肌直径(cm)=- 0.154+0.034×胎龄;肛门括约肌周长(cm)=- 0.139+0.117×胎龄;肛门括约肌面积(cm2)= - 0.776+ 0.055×胎龄。异常组48例产前诊断肛门闭锁胎儿在不同孕周上述各测值均为0。
讨论
肛门闭锁可以单独发生,也可伴发于尾部退化综合征或作为多种复杂综合征的一部分。此外,孕母肥胖和糖尿病也能增加胎儿肛门闭锁发生的风险。在孕6~7周,尿囊与后肠之间的间充质增生,由头侧向尾侧或由两侧向中线生长,形成突入泄殖腔的镰状隔膜,称尿直肠隔。
后肠尾段膨大称为泄殖腔,其末端内胚层与表面的外胚层紧密相贴形成泄殖腔膜。尿囊从泄殖腔延伸至脐带,泄殖腔膜被分为腹侧的尿生殖膜和背侧的肛膜。肛膜的外侧为一浅凹,称肛凹或原肛。肛膜通常于孕7~8周破裂,肛门闭锁因肛膜未破或肛凹形成障碍所致。
自1978年Bean等首次产前超声诊断肛门闭锁以来,相继有肛门直肠畸形超声诊断的报道出现,主要根据肛门闭锁近段结肠或直肠肠管扩张作为诊断依据推断出来,不出现肠管扩张者,产前超声检查困难。造成上述肠管扩张的一种可能机制是肛门闭锁并发直肠尿道瘘,使胎儿尿液反流进入肠管所致。
然而,伴直肠尿道瘘的肛门闭锁发生率较低,仅为15.9%-42.O%,这也解释了采用超声发现肠管扩张作为肛门闭锁的标准容易出现漏诊或误诊的可能原因。此外,最近有作者认为胎儿肛门括约肌缺失可能是产前诊断肛门闭锁的一种可能方法。在健康孪生胎儿肛门声像图呈现“靶环征”,而另- VACTERL联合征胎儿没有显示肛门“靶环征”。
正常胎儿肛门“靶环征”是胎儿肛门横切面上的典型表现。肛管周围有肛门内、外括约肌,肛门内括约肌是一厚的环形平滑肌管;肛门外括约肌是一骨骼肌管,位于肛管肌外层,围绕整个肛管。
肛门括约肌在声像图上表现为较厚的圆形低回声,中央高回声点是由黏膜组织形成的反射回声,周围圆形高回声是肛门括约肌外层与周围组织形成的界面反射,共同形成了高一低一高的同心圆样回声,呈靶环样排列,称之为“靶环征”或“同心圆征”。从图1,2可以发现当声束从胎儿左侧或右侧入射时,胎儿肛门“靶环征”图像清楚,层次分明。当声束从胎儿背侧或腹侧入射时,胎儿肛门“靶环征”图像较模糊,层次欠清。
因此,建议产前观察胎儿肛门部“靶环征”时超声声束尽量从胎儿左侧或右侧入射。肛门闭锁肛门横切面声像图表现为一高或低的线状回声(图3,4)。当超声声束从胎儿腹侧或背侧进入时,由于没有反射界面,声波不能反射回来,所以在声像图上表现为一线状低回声;当超声声束从胎儿左侧或右侧进入时,声波可通过反射界面反射回来,因而在声像图上表现为一线状高回声。
本研究以大样本的孕18~40周胎儿作为研究对象,全面评价正常胎儿肛门“靶环征”各项参数,并将肛门闭锁胎儿的肛门测值进行比较。研究发现813例正常胎儿中,755例肛门括约肌声像图呈现“靶环征”,显示率高达92.7%(755/813)。其中9例胎儿产前超声发现肠管扩张而怀疑肛门闭锁,通过“靶环征”排除该诊断,产后追踪观察均能正常排便得以证实。
58例胎儿(孕周>37周或孕周<21周)显示不清,考虑与会阴部受胎儿大小、肢体、子宫壁及胎盘等体位因素的影响有关,由于不能显示肛门横切面而不能发现“靶环征”,这些病例也同样不能发现胎儿肛门部的线状回声。在“靶环征”切面上,进一步测量其直径、周长和面积以评估不同孕周胎儿肛门括约肌的发育情况。
笔者发现肛门括约肌直径、周长和面积与孕周呈线性正相关,随着孕周时间的延长,各测值逐渐增加。本研究与近期国外学者的系列研究结果相似。同时,在研究中还发现产前超声检查“靶环征”的最佳孕周为21~37周,此时期“靶环征”的显示率高达97%~100%,这与解剖学上肛门外括约肌的发育时间基本相符。
本研究中48例肛门闭锁胎儿经产前肛门超声检查均不能显示肛门“靶环征”。因此,在产前超声诊断肛门闭锁时,胎儿肛门横切面“靶环征”的图像显示与观察可能具有重要的价值。然而,未发现肛门括约肌直径、周长和面积测值与诊断肛门闭锁的可能量化关系,48例肛门闭锁胎儿均为产前通过超声观察肛门“靶环征”的有或无作出判断。对于潜在的肛门括约肌发育不良胎儿是否可通过上述测值作出评估,且三者特异性、敏感性的差异如何,有待今后进一步探讨。
综上所述,笔者认为“靶环征”可能是产前超声筛查肛门闭锁的一种良好方法。当产前怀疑肛门闭锁时,细致观察胎儿肛门横切面以期超声显示肛门“靶环征”是不错的选择。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#产前超声#
44
#肛门#
63
#产前#
49
#超声诊断#
68
#超声诊断#
80