PLoS Pathog:P物质引起猪肉绦虫感染患者的癫痫发作
2012-02-15 MedSci MedSci原创
贝勒医学院的研究人员在一篇发表于网上开放存取期刊PLoS Pathogens上的报道中说,一种称为P物质的神经肽是导致大脑被猪肉绦虫(Taenia solium)感染的癫痫患者发作。 "神经囊虫病或大脑绦虫寄生虫感染,是获得性癫痫的主要原因",此报道的通讯作者、感染病医学副教授Prema Robinson博士说,"为了开发治疗或预防它们,理解这些癫痫的来源尤其重要。" P物质是一种神经肽(一个

贝勒医学院的研究人员在一篇发表于网上开放存取期刊PLoS Pathogens上的报道中说,一种称为P物质的神经肽是导致大脑被猪肉绦虫(Taenia solium)感染的癫痫患者发作。
"神经囊虫病或大脑绦虫寄生虫感染,是获得性癫痫的主要原因",此报道的通讯作者、感染病医学副教授Prema Robinson博士说,"为了开发治疗或预防它们,理解这些癫痫的来源尤其重要。"
P物质是一种神经肽(一个涉及神经元间间交流的小蛋白样分子)。它由神经元、内皮细胞(排列于血管的细胞)和参与宿主防御反应的细胞所产生。在20世纪30年代被发现,长时间以来被认为是一个痛苦递质。然而,近年来,它也被发现在许多其他功能中发挥作用。
大脑炎症
Robinson认识到P物质参与炎症过程,并想知道它是否涉及癫痫发作活动。
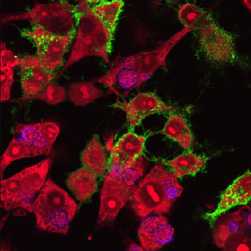
Robinson和她的包括一个来自波士顿塔夫茨大学医学中心同事在内的同事,在绦虫感染病人尸体的大脑中发现P物质。他们在未感染的大脑中没有发现P物质。
"只要寄生虫活着,就没什么发生", Robinson说。但是,一旦蠕虫死亡,机体与招募免疫系统细胞到感染部位的化学物质发生反应,这就引起炎症。她的研究表明,发现产生P物质的细胞主要在死虫附近的炎症区。
她说,给动物单独注射P物质或注射感染小鼠内蠕虫附近炎症区域(肉芽肿)提取物,它会患严重的癫痫发作。
当啮齿类动物接受阻断P物质受体的药物,它们不会癫痫发作。
此外,缺乏P物质受体的小鼠即使注射感染小鼠肉芽肿提取物也不癫痫发作。另外,缺少制造P物质细胞的小鼠的肉芽肿提取物不会诱导癫痫发作。
阻断受体的药物
她说,这些发现影响那些在绦虫感染治疗期间经常遭受癫痫发作的人。当蠕虫死亡,炎症细胞急涌入现场,癫痫发作开始。有阻断P物质受体的已知药物。这些药物可以证明是治疗和预防这些病人癫痫发作用的最有效方法。
Robinson计划在诸如癌症和结核病一样的与癫痫发作相关的其他疾病中观察P物质可能发挥的作用。
参与她的研究的其他人包括:Armandina Garza, Jose A. Serpa, Jerry Clay Goodman, Kristian T. Eckols, Bahrom Firozgary和David J. Tweardy,他们都来自贝勒医学院,再加上塔夫茨大学医学中心的Joel Weinstock。
这项工作的资金来自NIH的资助。
Substance P Causes Seizures in Neurocysticercosis
Prema Robinson, Armandina Garza, Joel Weinstock, Jose A. Serpa, Jerry Clay Goodman, Kristian T. Eckols, Bahrom Firozgary, David J. Tweardy
Abstract Neurocysticercosis (NCC), a helminth infection of the brain, is a major cause of seizures. The mediators responsible for seizures in NCC are unknown, and their management remains controversial. Substance P (SP) is a neuropeptide produced by neurons, endothelial cells and immunocytes. The current studies examined the hypothesis that SP mediates seizures in NCC. We demonstrated by immunostaining that 5 of 5 brain biopsies from NCC patients contained substance P (SP)-positive (+) cells adjacent to but not distant from degenerating worms; no SP+ cells were detected in uninfected brains. In a rodent model of NCC, seizures were induced after intrahippocampal injection of SP alone or after injection of extracts of cysticercosis granuloma obtained from infected wild type (WT), but not from infected SP precursor-deficient mice. Seizure activity correlated with SP levels within WT granuloma extracts and was prevented by intrahippocampal pre-injection of SP receptor antagonist. Furthermore, extracts of granulomas from WT mice caused seizures when injected into the hippocampus of WT mice, but not when injected into SP receptor (NK1R) deficient mice. These findings indicate that SP causes seizures in NCC, and, suggests that seizures in NCC in humans may be prevented and/or treated with SP-receptor antagonists.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








如何在临床癫痫发作病人检测P物质
90
#猪肉绦虫#
48
#猪#
33
#绦虫#
36