在65岁以上的住院病人中,有高达40%的人受到谵妄的影响,并与死亡几率增加3倍有关,但导致谵妄的神经机制仍然是未知的。谵妄和痴呆是截然不同但相互关联的认知障碍的原因。痴呆症是谵妄的一个强有力的风险因素。谵妄可以独立地预测新发痴呆症,而且接触谵妄的机会增加与认知结果不佳有关。尽管谵妄表明易患痴呆症,但谵妄期间神经轴损伤的证据支持谵妄和痴呆症之间存在因果关系的可能性。因此,研究谵妄的神经生物学并确定治疗目标,不仅有可能改善谵妄患者的预后,还能减少全球痴呆症的负担。
由于谵妄和痴呆在流行病学和临床上的重叠,研究它们共同的病理生理机制具有临床意义。然而,组织病理学研究表明,谵妄后的认知能力下降是由机制上独特的途径造成的,而不是那些与痴呆症有关的经典途径,如淀粉样斑块、神经纤维缠结和血管损伤。此外,针对这些传统痴呆病症的药物临床试验未能改变痴呆的发展轨迹,因此必须探索谵妄和痴呆研究的其他途径。大脑葡萄糖代谢低下是痴呆症的一个核心特征。
18F-氟脱氧葡萄糖正电子发射断层扫描(FDG-PET)上的低代谢模式可以帮助诊断痴呆症,预测从基线认知到轻度认知障碍(MCI)以及从MCI到阿尔茨海默病(AD)的进展。FDG是一种葡萄糖类似物,它的摄取是葡萄糖代谢的替代性测量。FDG摄取率是神经和突触活动的一个可靠指标。
大脑葡萄糖代谢低下,以及作为一种生物标志物,在AD的病理生理学中起着重要作用。针对人类脑部生物能量途径的临床试验已经显示出一些有希望的早期结果。
大脑代谢不足也是谵妄的一个特征。老年谵妄患者的脑脊液(CSF)中乳酸含量增加,关键碳水化合物酶的含量改变,表明有氧代谢受到抑制。由于区域性脑灌注与葡萄糖的利用相联系,神经影像学研究也表明,谵妄期间可逆的脑灌注不足、脑氧饱和度下降和自动调节功能失调,从而表明代谢的改变。
有两项研究使用FDG-PET来评估谵妄期间的葡萄糖代谢,都发现了皮质的低代谢。然而,在这两项研究中,痴呆症和急性疾病可能是重要的混杂因素。
在这项探索性研究中,澳大利亚新南威尔斯大学的Anita Nitchingham等人, 试图确定大脑葡萄糖代谢低下的任何部分是否主要归因于谵妄而不是急性疾病或痴呆。他们用FDG-PET来比较有谵妄但没有痴呆症诊断或症状的不适患者与没有谵妄但同样没有痴呆症的急性不适对照组。
他们使用18F-氟脱氧葡萄糖正电子发射断层扫描(FDG-PET)评估了患有或不患有谵妄的老年病人的大脑葡萄糖代谢情况,所有病人都没有临床痴呆(N = 20)。采取了严格的排除标准,以尽量减少既定混杂因素对FDG-PET的影响。
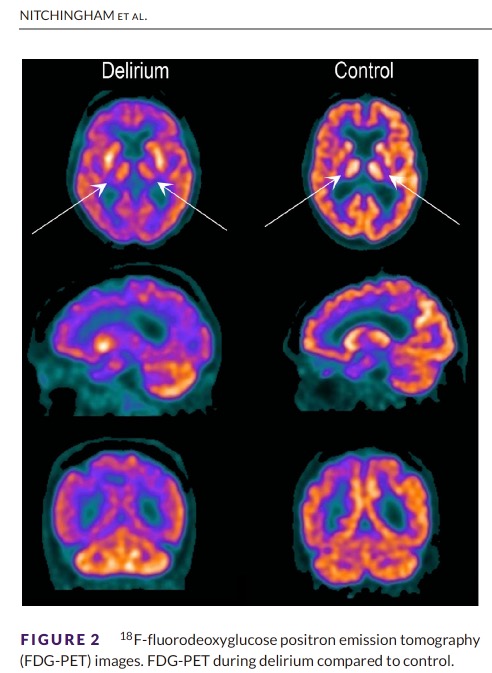
他们发现:谵妄患者的双侧丘脑和右上额、右后扣带回、右内外侧前颞和左上顶叶皮层显示出低代谢。
区域代谢低下与谵妄的严重程度和神经心理学测试的表现相关。
该研究的重要意义在于发现了:在患有急性疾病但没有临床痴呆的患者中,谵妄伴随着区域性脑代谢低下。虽然一些低代谢区域可能代表临床前阿尔茨海默病(AD),但丘脑的低代谢是不典型的AD,与谵妄特有的临床特征一致。
原文出处:
Nitchingham A, Pereira JV, Wegner EA, Oxenham V, Close J, Caplan GA. Regional cerebral hypometabolism on 18F‐FDG PET/CT scan in delirium is independent of acute illness and dementia. Alzheimer’s & Dementia. Published online March 15, 2022:alz.12604. doi:10.1002/alz.12604
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#alzheimers#
43
#dementia#
38
谵妄病人怎么配合做的PET,好奇
43
#ERS#
37
坚持学习
51
#MERS#
51