Prostate Cancer P D:新诊断转移性前列腺癌放射治疗的长期结果
2021-04-25 AlexYang MedSci原创
在转移性前列腺癌患者中,局部治疗的作用在不断发展。近期报道的两项大规模随机试验表明,针对前列腺的放疗可提高低转移负荷患者的总生存(OS)。
在转移性前列腺癌患者中,局部治疗的作用在不断发展。近期报道的两项大规模随机试验表明,针对前列腺的放疗可提高低转移负荷患者的总生存(OS)。

最近,有研究人员回顾了他们中心在这种背景下的前列腺放射治疗经验。
研究包括了2005年至2015年期间转诊到一个综合癌症中心的新诊断的转移性激素敏感前列腺癌(mHSPC)男性,他们最初接受雄激素阻断疗法。研究队列包括了410名患者,其中128人接受了前列腺RT。随访中位数为61.0个月。在单变量分析中,接受前列腺RT与OS的改善有关(HR 0.59,95%CI 0.45-0.77,p=0.0001)。接受前列腺RT的患者的OS中位数为47.4个月,而未接受前列腺RT的患者为26.3个月。在多变量Cox模型中,接受前列腺RT仍与OS改善有关(HR 0.69,95%CI 0.50-0.94,p=0.02)。另外,在接受前列腺RT治疗的患者中,BED的增加也与OS的改善有关(HR 0.87,每增加10Gy,95%CI 0.76-0.99,p=0.03)。
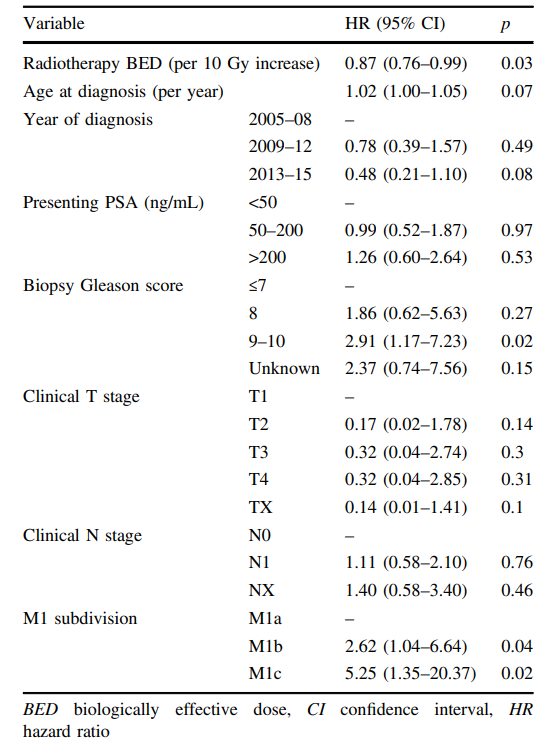
接受放疗患者的总生存多变量Cox模型(n=128)
最后,研究人员指出,他们的队列代表了迄今为止报道的最大的单中心原发肿瘤定向RT治疗mHSPC的经验。在该人群中,接受前列腺RT与OS的改善有关,OS获益的程度具有临床意义。因此,RT剂量响应梯度的情况也值得进一步研究。
原始出处:
Scott C Morgan, Oliver E Holmes , Julia Craig et al. Long-term outcomes of prostate radiotherapy for newly-diagnosed metastatic prostate cancer. Prostate Cancer P D. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Prostate Ca#
43
#长期结果#
42
#新诊断#
33
已经写进指南了
53
#ROS#
35
#转移性#
25
#转移性前列腺癌#
44
#PRO#
23
前列腺癌相关研究,学习了,谢谢梅斯
54