Gastric Cancer: D1/D2和CRITICS研究事后探索可手术不同分子亚型胃癌对新辅助化疗的应答和预后
2022-02-19 yd2015 MedSci原创
研究表明,在可切除的胃癌中,与EBV- /MSS亚型相比,MSI-high亚型患者具有良好的预后,无论是在手术治疗的患者中,还是在接受围手术期化疗(放射)治疗的患者中。
Epstein - Barr病毒感染(EBV+)和高度微卫星不稳定性(MSI-high)是可切除胃癌(GC)患者生存的预后良好因素。然而,MSI-high的肿瘤患者围手术期治疗的益处仍然是一个讨论的话题。近期,Gastric Cancer杂志上发表一项相关研究成果,主要是探索仅接受手术治疗或围手术期治疗的EBV+、MSI-high和EBV- /MSS GCs患者的临床病理结果。

研究纳入D1/D2研究中接受手术治疗的447名患者,而在CRITICS研究中,纳入451名接受围手术期治疗患者,通过肿瘤样本来确定EBV和MSI状态。探索病理应答、肿瘤形态特征和生存率的相关性。
在D1/D2研究中,47(10.5%) 例患者 为EBV+ ,47 (10.5%)例患者为MSI-high,353(79.0%)例患者为EBV- /MSS。而在CRITICS研究中,25 (5.5%)例患者为EBV+ ,27 (5.9%) 例患者为MSI-high,402(88.5%)例患者为EBV- /MSS。


在D1/D2研究中,EBV+患者的5年肿瘤相关死亡率(CRS)为65.2%,MSI-high患者为56.7%,EBV -/MSS患者为47.6% (与EBV−/MSS患者相比,EBV+患者的HR=0.57, 95 CI 0.31-0.99, P = 0.047;MSI-high患者的HR=0.78, 95%CI 0.48-1.27, P = 0.32)。EBV+患者的5年OS率为51.1%,MSI-high患者为46.8%,EBV−/MSS患者为42.5% (与EBV−/MSS患者相比,EBV+患者的HR=0.90, 95% CI 0.63-1.30, P = 0.59, MSI-high患者为HR=1.31, 95% CI 0.92-1.82, P = 0.10)。

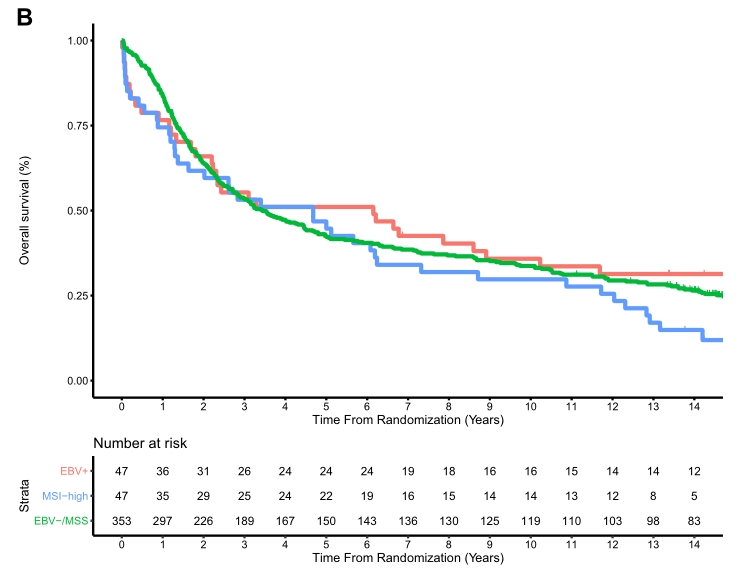
D1/D2研究不同亚型CRS和OS差异
在CRITICS研究中,与EBV−/MSS患者相比,EBV+患者的5年CRS为69.8%,MSI-high患者的为51.7%,EBV-/MSS患者为38.6% (与EBV−/MSS患者相比,EBV+患者的HR=0.44, 95% CI 0.22 -0.88, P = 0.02;MSI-high患者的HR=0.67, 95 CI 0.37-1.19, P = 0.17)。EBV+患者的5年OS率为56.0%,MSI-high患者为51.3%,EBV - /MSS患者为36.7% (与EBV−/MSS患者相比,EBV+患者的HR=0.64, 95% CI 0.36-1.11, P = 0.11;MSI-high患者的HR=0.67, 95% CI 0.39-1.14, P = 0.14)。
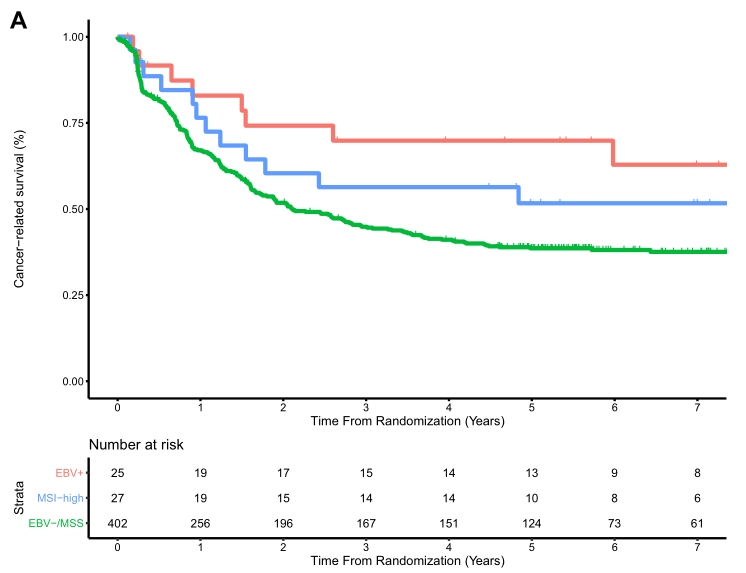
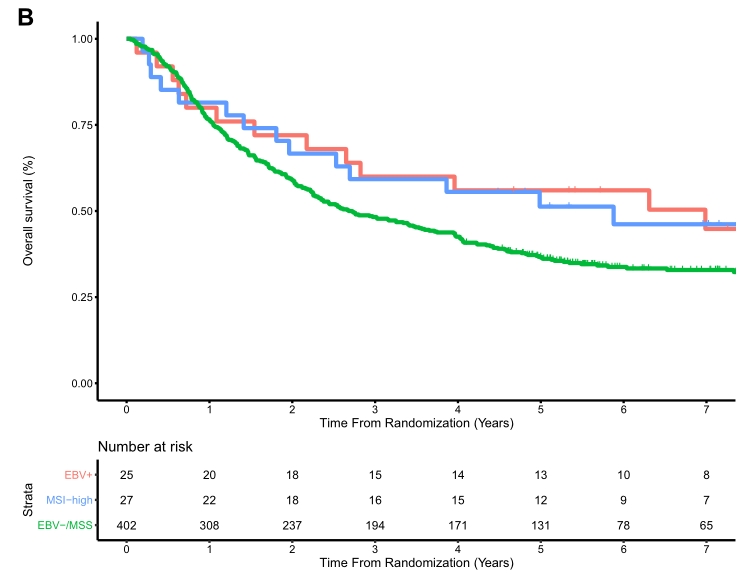
CRITICS研究不同亚型CRS和OS差异
在CRITICS研究中,2例MSI-high患者新辅助化疗后显示(接近)完全的组织病理缓解(TRG1-2)。5例EBV+肿瘤显示(接近)完全的组织病理应答(TRG1-2)。9/36例(25.0%)EBV -/MSS患者出现TRG 1-2。
综上,研究表明,在可切除的胃癌中,与EBV- /MSS亚型相比,MSI-high亚型患者具有良好的预后,无论是在手术治疗的患者中,还是在接受围手术期化疗(放射)治疗的患者中。
原始出处:
Biesma HD, Soeratram TTD, Sikorska K, Caspers IA, van Essen HF, Egthuijsen JMP, Mookhoek A, van Laarhoven HWM, van Berge Henegouwen MI, Nordsmark M, van der Peet DL, Warmerdam FARM, Geenen MM, Loosveld OJL, Portielje JEA, Los M, Heideman DAM, Meershoek-Klein Kranenbarg E, Hartgrink HH, van Sandick J, Verheij M, van de Velde CJH, Cats A, Ylstra B, van Grieken NCT. Response to neoadjuvant chemotherapy and survival in molecular subtypes of resectable gastric cancer: a post hoc analysis of the D1/D2 and CRITICS trials. Gastric Cancer. 2022 Feb 7. doi: 10.1007/s10120-022-01280-2. Epub ahead of print. PMID: 35129727.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#GAS#
42
#新辅助#
56
#gastric#
52
#AST#
39
#分子亚型#
46