盘点:近期骨髓瘤研究进展汇总
2017-02-25 MedSci MedSci原创
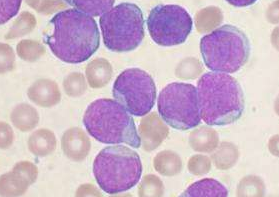
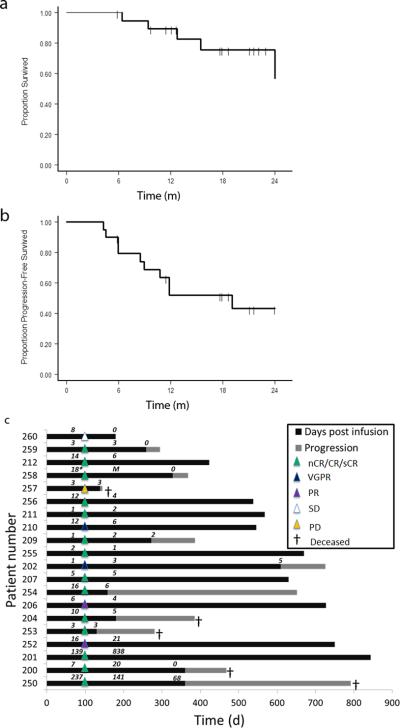
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里小M整理了近期关于骨髓瘤的重要研究新进展与各位一同分享。【1】JABFM:出现这些信号,要小心多发性骨髓瘤 根据美国家庭医学委员会杂志发表的一项研究结果显示,患者若出现异常的实验室检查结果、体重减轻或疲劳,临床医生应该警惕多发
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很全面的归纳,收藏了
60
#研究进展#
49
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了!
85
进展这么迅速
81
棒棒哦
74
骨髓瘤研究
80
顽固性疼痛、病理性骨折、脊柱不稳定、脊髓与神经根压迫症以及巨大软组织肿块等SRE的患者,化疗或(和)放疗作用十分有限,往往需要手术治疗。
35
好东西,收藏了
38
看看
33