HUMAN BRAIN MAPPING:右侧前海马形变与物质使用障碍遗传风险有关
2022-04-14 影像小生 MedSci原创
FH+青少年右前海马体内向变形可能与FH+后代行为失调导致SUD的风险增加有关
物质使用障碍(SUD)在具有家族史(FH)的SUD (FH+)个体中普遍存在,这种SUD风险的增加很可能通过复杂的遗传和环境/学习机制传播。然而,这种传递的神经相关性仍然知之甚少,部分原因是很难区分家庭传递和物质使用导致的神经特征。虽然皮质下结构(subcortical structures, SSS)的体积和形状已被证明是可遗传的,但这些结构,特别是苍白球、壳核、伏隔核和海马体,也与物质使用障碍有关。然而,尚不清楚这些解剖差异是先于药物使用还是药物使用的结果。
Zhishun Wang等在HUMAN BRAIN MAPPING杂志发表题为Shapes of subcortical structures in adolescents with and without familial history of substance use disorder的文章,研究了具有SUD家族史(FH+)的青少年的体积和SSS是否与没有此类家族史(FH-)的青少年不同。

由于SUD的风险与焦虑和冲动有关,他们还研究了这些心理特征与体积/SSS之间的相关性。该研究利用结构MRI和FSL软件对皮质下结构进行分段,获得64例FH+和58例FH-青少年的SSS和体积指标。研究了体积和SSS的组间差异,以及体积/SSS与特质焦虑和冲动性之间的相关性。
该研究发现
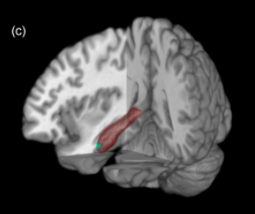
- 与FH-青少年相比,FH+青少年右前海马体的形状有明显的内向变形,而该结构的体积没有组间差异。
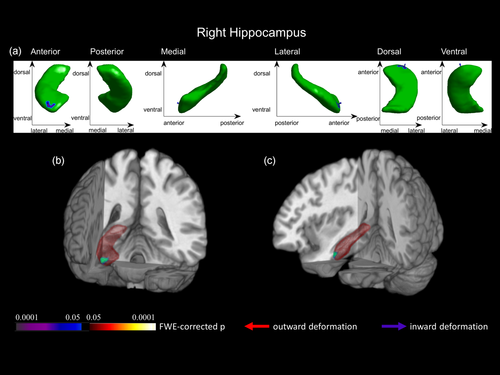
FH+组与FH-组海马形状分析结果
其他皮层下结构的形状和体积均无组间差异。
- FH+青少年左海马形状与特质焦虑和冲动性均呈正相关,而FH+青少年海马形状与SSS呈负相关。
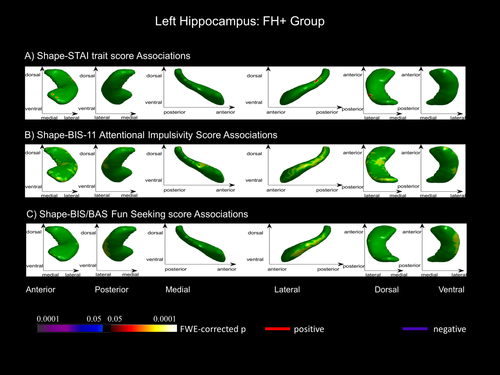
FH+组形状-行为得分相关分析
该研究团队认为SSS似乎可以捕捉到传统容量分析无法捕捉到的局部解剖特征。
Zhishun Wang的研究证明FH+青少年右前海马体内向变形可能与FH+后代行为失调导致SUD的风险增加有关。海马形状在FH+和FH-青少年的焦虑和冲动得分中也表现出相反的相关模式。这些新发现可能揭示了传统容量分析未能捕捉到的SUD家族性易感性增加的神经相关性。这表明皮层下形状分析似乎比传统体积分析更能捕捉解剖-临床相关性。重要的是,由于SSS表现出很强的遗传性,但对环境因素也很敏感,这些影像学结果可能代表了SUD风险家族传播的神经相关因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mapping#
49
#物质使用障碍#
52
#human#
52
#遗传风险#
53