J Hypertens:主动脉缩窄修复的儿童颈动脉内膜中层厚度增加与血压升高有关
2019-04-06 xing.T 网络
由此可见,cIMT与儿童BMI的z评分、男性和CoA修复呈正相关。修复CoA的儿童cIMT增加是因为血压异常升高,大多数患者在临床上都被掩盖了。这些发现值得进一步研究cIMT和其他动脉粥样硬化危险因素,以确定它们对这些高度易感患者的潜在临床影响。
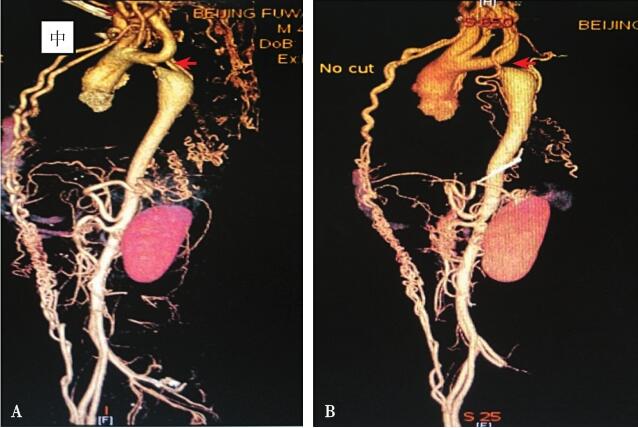
颈总动脉(cIMT)内膜中层厚度是心血管疾病一个良好的无创替代指标,对先天性心脏病患儿进行定期cIMT监测具有很大的价值。近日,高血压领域权威杂志Journal of Hypertension上发表了一篇研究文章,研究人员试图确定哪些拟人变量和血液动力学变量与肥胖儿童患者和修复的主动脉缩窄儿童(CoA)cIMT显著相关。
研究人员测量了143名5岁至18岁以下儿童cIMT,包括正常体重对照者(n=44),超重/肥胖儿童(n=73)和修复CoA的儿童(n=26)。比较cIMT,并研究cIMT与患者特征(包括肥胖和血压(BP))之间的关联。
BMI的z评分、性别和CoA是cIMT的重要独立预测因子。超重/肥胖儿童的cIMT(0.53±0.06 mm)显著高于正常体重对照者(0.51±0.04 mm),与正常BP的CoA患者(0.52±0.05mm)和对照者(0.51±0.04mm)相比,异常高血压的CoA患者(0.57±0.08 mm)也是如此。血压正常的CoA患者cIMT没有显著增加。
由此可见,cIMT与儿童BMI的z评分、男性和CoA修复呈正相关。修复CoA的儿童cIMT增加是因为血压异常升高,大多数患者在临床上都被掩盖了。这些发现值得进一步研究cIMT和其他动脉粥样硬化危险因素,以确定它们对这些高度易感患者的潜在临床影响。
原始出处:
Dempsey, Adam A.et al.Increased blood pressure is associated with increased carotid artery intima–media thickness in children with repaired coarctation of the aorta.Journal of Hypertension. 2019.https://journals.lww.com/jhypertension/Abstract/publishahead/Increased_blood_pressure_is_associated_with.97230.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血压升高#
30
#主动脉缩窄#
41
#颈动脉#
31
#内膜#
28
#PE#
28
#TENS#
42
#主动脉#
30
#颈动脉内膜中层厚度#
32