AJRCCM:心脏MRI在评估肺动脉高压危险分层中的作用
2021-10-28 刘少飞 MedSci原创
心脏磁共振成像 (MRI) 是评估右心室功能的金标准测试,对肺动脉高压具有预后作用。心脏 MRI 可以识别高比例的 1 年死亡率低风险患者,并且在与当前的风险分层方法结合使用时可以改善风险分层。

肺动脉高压 (PAH) 是一种罕见且会缩短寿命的疾病。未经治疗,预期寿命不到 3 年,但经过治疗,特发性 PAH 患者的 5 年生存率超过 60%。欧洲心脏病学会和欧洲呼吸学会 (ESC/ERS) 指南提出了“红绿灯”风险分层评分,以帮助医生做出治疗决策,将患者分类为低风险(“绿色”,<5%)、中等风险(“琥珀色”,5-10%),或基于许多可修改变量的 1 年死亡率高风险(“红色”,>10%)。尽管用于这些变量的阈值主要基于专家意见,但它们已在三个欧洲注册处得到验证。这些研究表明,在随访中改善至低风险的患者比没有改善的患者有更好的结果。留在中危组的患者的预后明显低于低危患者,目前的方法旨在改善和维持低危组的患者。
风险分层方法通常包括多个变量;然而,右心室功能被认为是 PAH 发病率和死亡率的主要决定因素。心脏磁共振成像 (MRI) 是公认的评估右心室功能的金标准。尽管超声心动图更广泛、更便宜并且是右心室评估最常用的成像方式,但由于缺乏观察者间和观察者内的可重复性和声窗,而受到限制。因此,本研究试图确定心脏 MRI 指标是否可以使用三个风险级别的 ESC/ERS 标准准确地对患者进行风险分层,以及是否可以使用阈值来帮助风险分层。
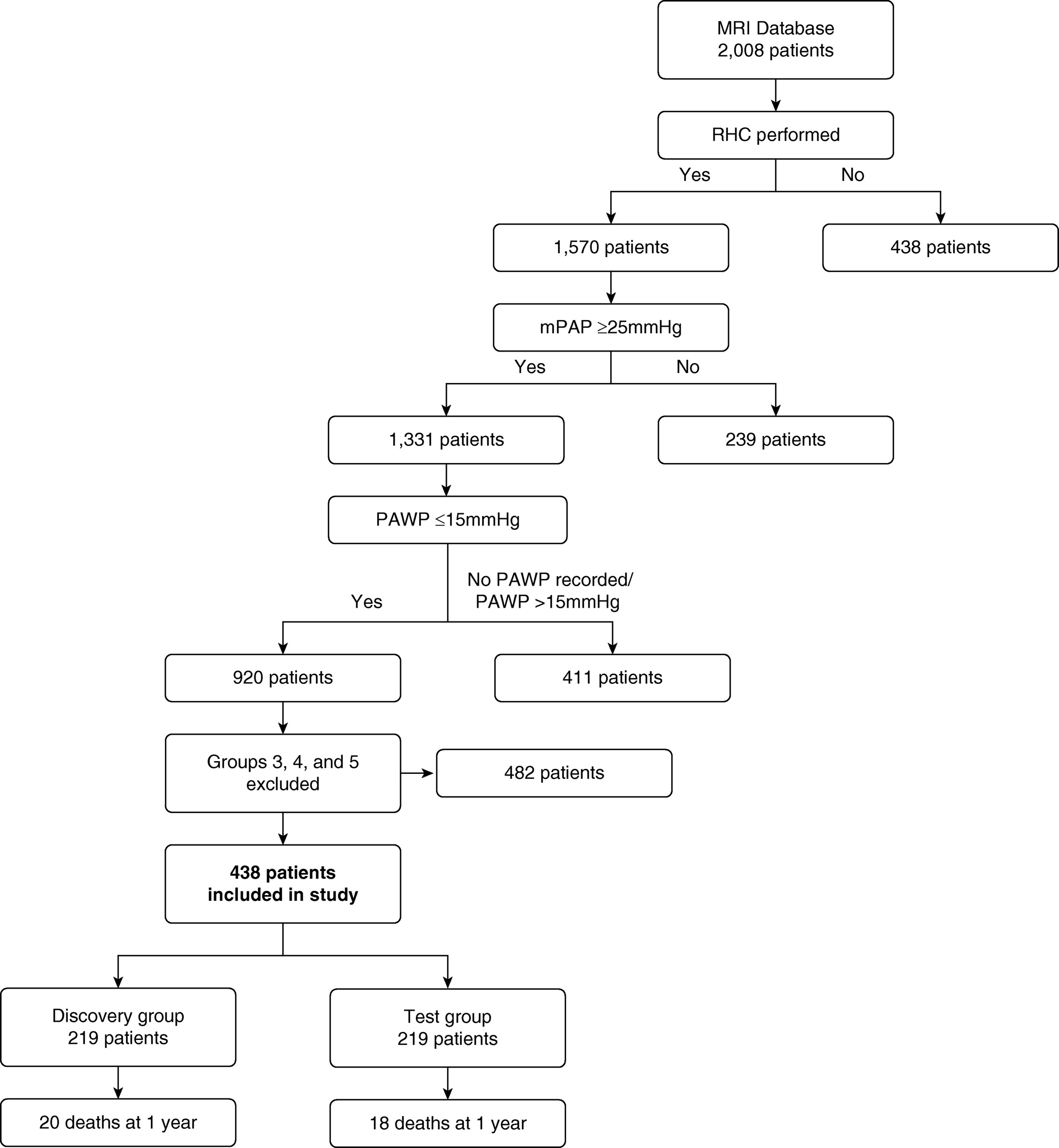
研究队列:流程图显示包括的患者和排除的原因
心脏 MRI 后 1 年,38 名患者(8.7%)死亡; 20 名患者 (9.1%) 在发现队列中,18 名患者 (8.2%) 在测试队列中。 年龄大于 50 岁的患者更可能在 1 年时死亡(P = 0.008),PAH 与结缔组织病相关的患者也是如此(P = 0.001)。
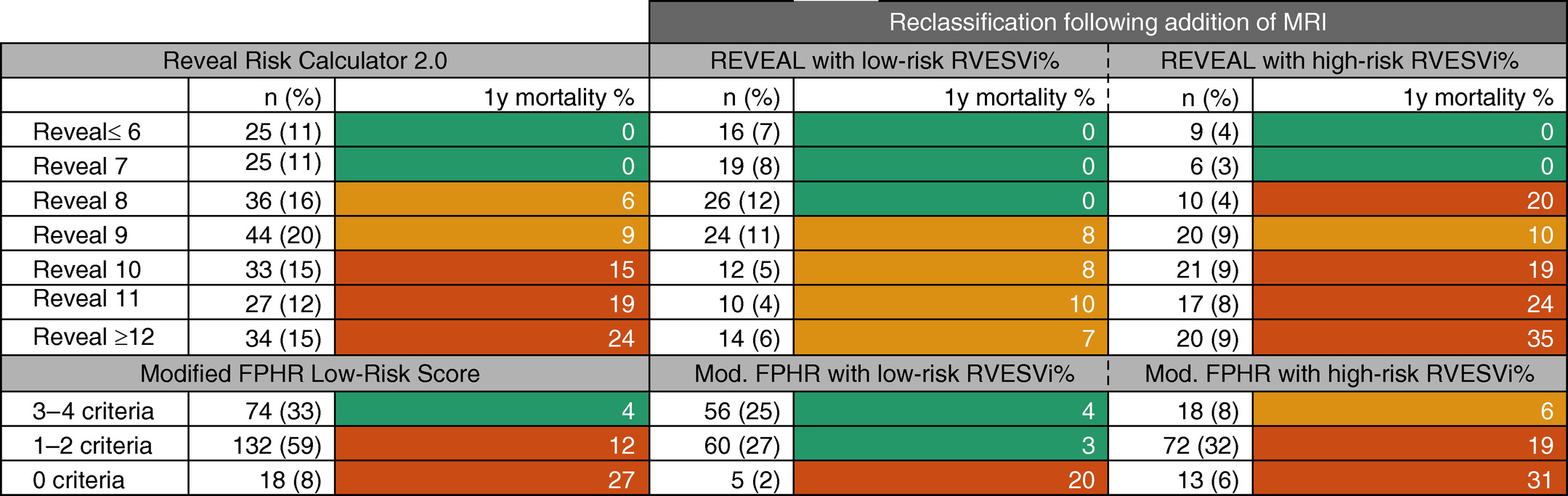
该研究评估了如何将心脏 MRI 与当前的风险分层方法结合使用;当与 REVEAL 2.0 和改良的 FPHR 结合使用时,百分比预测的 RVESVi 能够进一步对患者进行风险分层。 对于根据改良 FPHR 归类为低风险或 REVEAL 2.0 风险评分≤6 的患者,MRI 不影响风险分层。 然而,当与 REVEAL 2.0 风险计算器结合使用并使用 +2 或 -2 分的二分评分来预测 RVESVi 阈值为 227% 时,对于 REVEAL 2.0 评分 >6 的患者,MRI 能够重新分类 36% 的患者进入低风险组,11% 的患者进入高风险组。
基于 REVEAL 2.0 风险评分 ≤6 为低风险,7 至 8 为中风险,≥9 为高风险并使用 +2 或 -2 的二分评分来表示 227% 的百分比预测 RVESVi 阈值, MRI 将 47% 的患者重新分类:36% (n = 82) 为低风险组,11% (n = 25) 为高风险组。
对于 REVEAL 2.0 风险评分,对于百分比预测的 RVESVi ≥ 227% 和 <227% 分别加减 2 分,使 C 统计值从 0.74(95% CI, 0.65–0.83) 到 0.78(95% CI,0.70–0.87)。 使用改进的 FPHR 方法,C 统计量从 0.70(95% CI,0.59-0.80)增加到 0.74(95% CI,0.63-0.84),为百分比预测 RVESVi <227% 的患者增加一个额外的点。
源自心脏 MRI 指标的阈值可用于对 PAH 患者进行风险分层。 该注册表明,心脏 MRI 在用作唯一的风险分层工具时,可识别出 1 年死亡率低风险的患者比例很高,并且当与当前的风险分层方法结合使用时,可以改善风险分层。
文章出处:
Lewis RA, Johns CS, Cogliano M, Capener D, Tubman E, Elliot CA, Charalampopoulos A, Sabroe I, Thompson AAR, Billings CG, Hamilton N, Baster K, Laud PJ, Hickey PM, Middleton J, Armstrong IJ, Hurdman JA, Lawrie A, Rothman AMK, Wild JM, Condliffe R, Swift AJ, Kiely DG. Identification of Cardiac Magnetic Resonance Imaging Thresholds for Risk Stratification in Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2020 Feb 15;201(4):458-468. doi: 10.1164/rccm.201909-1771OC. PMID: 31647310; PMCID: PMC7049935.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#危险分层#
35
#RCC#
29
#动脉高压#
35
很好
63
棒
58
yyds
41
#心脏MRI#
50