JAHA:颈动脉粥样硬化可预测高血压患者的血压控制情况
2022-01-20 MedSci原创 MedSci原创
接受降压治疗的高血压患者出现CP与随访期间血压控制不佳相关,但与较差的代谢特征和左心室肥厚无关。
2018年欧洲心脏病学会/欧洲高血压学会-动脉高血压指南不推荐将常规颈动脉超声检查作为识别高血压引起器官损伤的工具,除非患者有临床指征。然而,颈动脉斑块(CP)与动脉僵硬度增加密切相关,随着时间的推移会影响血压(BP)控制。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估首次就诊时存在CP的证据是否可以预测随访期间的血压控制情况。
研究人员从CSN登记处确定了6684名高血压患者,他们接受了完整的颈动脉超声检查,并根据受试者基线是否存在CP进行分类。最佳血压控制定义为随访期间诊室和家庭血压的平均血压分别<140/90mmHg和<135/85mmHg。
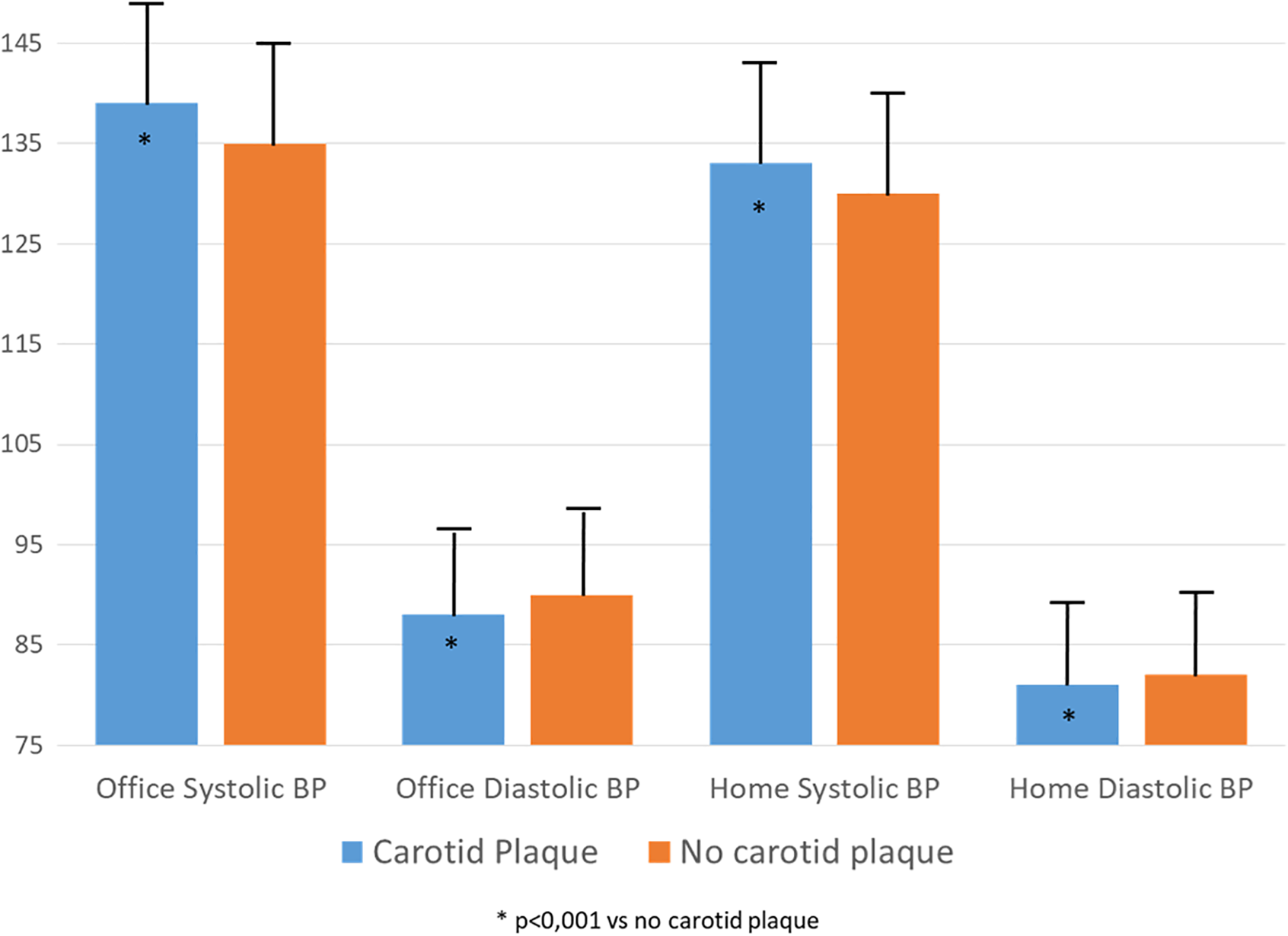
在基线时,伴有CP的参与者(n=3061)更有可能是男性、年龄较大、更有可能患有糖尿病,并且表现出更高的收缩压、更低的舒张压、更差的血脂参数和更高的左心室肥厚患病率(所有P<0.0001),相比于不伴有CP的患者。54%伴有CP和62%不伴有CP(P<0.0001)的参与者被判定达到了最佳诊室血压控制水平,51%伴有CP和58%不伴有CP(P<0.01)的参与者被判定达到了最佳家庭血压水平。CP的存在与随访期间达到诊室血压控制的可能性降低著着相关(所有P<0.0001),独立于年龄较大、男性、较高的基线血压值、药物类别和左心室伴有肥大的显著效应,并且仅因高血压持续时间而有所减弱。
由此可见,接受降压治疗的高血压患者出现CP与随访期间血压控制不佳相关,但与较差的代谢特征和左心室肥厚无关。
原始出处:
Costantino Mancusi.et al.Carotid Atherosclerosis Predicts Blood Pressure Control in Patients With Hypertension: The Campania Salute Network Registry.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.022345
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#颈动脉#
38
#粥样硬化#
53
#AHA#
51
#血压控制#
44
#高血压患者#
54
#颈动脉粥样硬化#
48