NEJM:鸟分枝杆菌复合体引起的腱鞘炎-病例报道
2019-12-19 xing.T MedSci原创
这些软组织肿块是由滑膜变性引起的纤维蛋白、胶原蛋白和细胞碎片的积聚所致。组织学分析显示为肉芽肿性腱鞘炎,分枝杆菌培养证实了由鸟分枝杆菌复合物引起的侵袭性分枝杆菌性腱鞘炎。
患者为一名51岁的右利手男子,因左手腕肿胀3年,进一步恶化,并伴有手指疼痛和麻木而就诊。他的病史包括2型糖尿病和人类免疫缺陷病毒感染。他坚持接受抗逆转录病毒疗法,他的CD4细胞计数为357每立方毫米。他没有手外伤或接受手术。
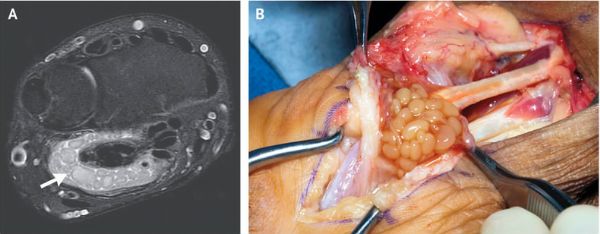
体格检查发现左手掌部略带紫色变。他四个手指的近端指间关节都有疼痛和伸展受限。磁共振成像(MRI)显示左腕掌侧尺骨囊液中有多个疏松体(“米体”)(如图A箭头所示)。该患者接受了彻底的腱鞘切除术,在此过程中,看到了与MRI上确定的米体相对应的软组织肿块(如图B所示)。
这些软组织肿块是由滑膜变性引起的纤维蛋白、胶原蛋白和细胞碎片的积聚所致。组织学分析显示为肉芽肿性腱鞘炎,分枝杆菌培养证实了由鸟分枝杆菌复合物引起的侵袭性分枝杆菌性腱鞘炎。
患者接受了利福布汀、乙胺丁醇和克拉霉素联合治疗;3个月后,由于副作用,停止了药物治疗。在5年的随访中没有复发的迹象。
原始出处:
Lucas Kreutz-Rodrigues,et al.Tenosynovitis Due to Mycobacterium avium Complex.N Engl J Med 2019;https://www.nejm.org/doi/full/10.1056/NEJMicm1901520
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#鸟分枝杆菌复合体#
38
#复合体#
42
#腱鞘炎#
48
#分枝杆菌#
40
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
53