
血管内血栓切除术(EVT)已被证明可以改善前循环大血管闭塞(LVO)导致的急性缺血性卒中患者的预后,在早期(0-6小时)和晚期(>6-24小时)的窗口期都有良好的影像学表现。
血管内血栓切除术的效果也与从最初成像到再灌注的时间成反比,尤其是在早期窗口期出现的患者,强调需要优化工作流程,加快患者到达血管内科的速度。许多患者最初在非血管内治疗中心就诊,需要转到血管内治疗中心,导致医院间转院时出现严重延误。为简化LVO患者到达具有EVT能力的中心所做的努力仍在不断发展,包括院前分流直接到具有EVT能力的中心,以及将患者从非EVT中心运送到EVT中心的最佳方法。同时,由于这些医院采用的流程和治疗方案,EVT中心可能会出现延误。尽量减少从到达EVT中心到血管造影室所需的时间,将继续在EVT效益最大化方面发挥重要作用。
在这个转移过程中,节省时间的方法之一是减少不必要的成像。通常在最初的非EVT中心至少获得1次非造影剂增强的计算机断层扫描(CT),对于在EVT中心到达后通过重复成像更精确地选择病人是否需要、是否值得花费额外的时间,或者如果病人直接转移到血管造影室(DTA方法),结果是否会更好,仍然存在不确定性。目前的指南并没有明确列出院间转院后在EVT中心重复成像的效用。
相反,考虑到院间转运过程中潜在的卒中演变,DTA是否安全还不得而知。此外,对于转院的LVO患者,重复造影的价值在早期(0-6小时)与晚期(>6-24小时)治疗窗的患者之间是否有差异,或者基于从非EVT中心造影到到达EVT中心的时间长度,也是未知数。另外,由于后勤和人员的不同,包括介入团队和卒中团队的现场服务,DTA的疗效和安全性可能会受到患者在工作时间内到达具有EVT能力的中心的影响。
藉此, The University of Texas McGovern Medical School的Amrou Sarraj等人,在整个研究人群和倾向性匹配的样本中,探究了被运送到有EVT能力的中心的患者的DTA的时间节省、有效性和安全性。
他们还评估了这些发现在早期和晚期治疗窗口之间以及在工作和待命时间之间是否存在差异。最后,评估了转院期间的时间(从到达转诊中心到到达EVT中心)以及从外部设施获取影像,到抵达EVT中心的时间与接受DTA的患者EVT的安全性和结果的关系,以及在某些亚组的患者中是否需要重复成像与转到EVT中心的时间有关。
这项在6个美国和欧洲综合卒中中心进行的集合性回顾性队列研究,招募了2014年1月1日至2020年2月29日期间患有前循环LVO(大脑内动脉或大脑中动脉分支M1/M2)并在最后已知井的24小时内转入EVT的成年人(年龄≥18岁)。
主要结局和措施:功能独立(90天修正的Rankin量表评分,0-2)是主要结果。症状性脑内出血、死亡率和时间指标也在DTA和重复成像组之间进行了比较。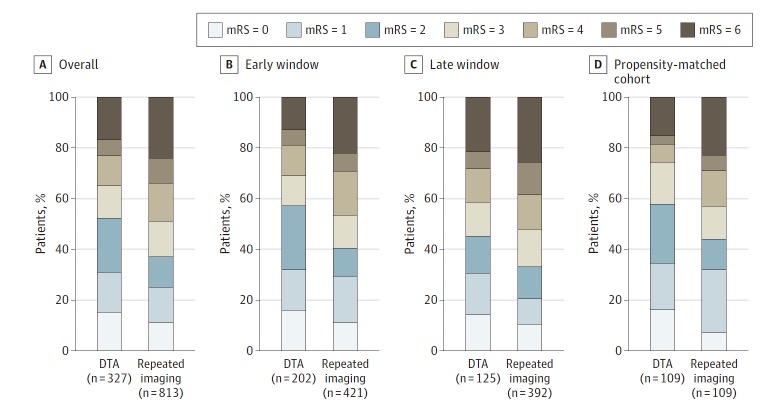
共有1140名LVO患者在转院后接受了EVT治疗,包括DTA组的327人(28.7%)和重复成像组的813人(71.3%)。中位年龄为69岁。529名女性,609名男性。
接受DTA的患者更多地使用了静脉阿替普酶(327例中的200例[61.2%]vs 808例中的412例[51.0%];P = .002),但其他组别则相似。
从到达EVT中心到腹股沟穿刺的中位时间,DTA更快,使用DTA的三个月功能独立性较高。
DTA的三个月死亡率较低。在重复成像组中,EVT中心到达腹股沟穿刺的时间增加10分钟与功能独立几率减少5%相关(aOR,0.95[95% CI,0.91-0.99];P = .01)。
在DTA组中,随着医院间转院时间超过3小时,改良的Rankin量表评分0至2分的比率下降,但在重复成像组中没有下降。
这个研究的重要意义在于:在所有时间和治疗窗口,DTA方法可能与更快的治疗和更好的功能结果有关。转移中的最佳EVT工作流程可能与更快、安全的再灌注有关,并能改善结果。
原文出处:
Sarraj A, Goyal N, Chen M, Grotta JC, Blackburn S, Requena M, Kamal H, Abraham MG, Elijovich L, Dannenbaum M, Mir O, Tekle WG, Pujara D, Shaker F, Cai C, Maali L, Radaideh Y, Reddy ST, Parsha KN, Alenzi B, Abdulrazzak MA, Greco J, Hoit D, Martin-Schild SB, Song S, Sitton C, Tsivgoulis GK, Alexandrov AV, Arthur AS, Day AL, Hassan AE, Ribo M. Direct to Angiography vs Repeated Imaging Approaches in Transferred Patients Undergoing Endovascular Thrombectomy. JAMA Neurol. 2021 Jun 14:e211707. doi: 10.1001/jamaneurol.2021.1707. Epub ahead of print. PMID: 34125153; PMCID: PMC8204255.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
46
#Neurol#
37
#血栓切除#
53
#血栓切除术#
50
#血管内血栓切除术#
42
不错啊
55
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
49
认真学习
52