Ann Rheum Dis:青年人血清尿酸水平与其高血压的发病存在相关性
2013-09-09 佚名 丁香园
A:男性血清尿酸水平超过345umol/l以后发生高血压风险升高 B:女性血清尿酸水平超过214umol/l以后发生高血压风险升高 研究要点: 1.本研究针对青年人的血清尿酸水平与高血压发病的相关性进行评估。 2.青年男性在血清尿酸水平超过345umol/l以后发生高血压的风险升高,尿酸水平每增加1mg/dl,其发生高血压的风险增加25%。
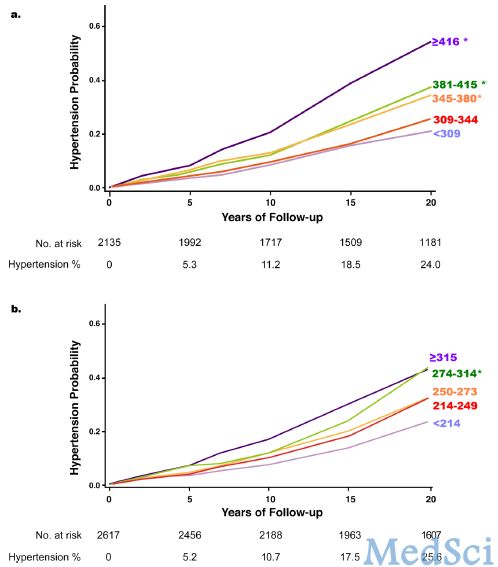
A:男性血清尿酸水平超过345umol/l以后发生高血压风险升高
B:女性血清尿酸水平超过214umol/l以后发生高血压风险升高
研究要点:
1.本研究针对青年人的血清尿酸水平与高血压发病的相关性进行评估。
2.青年男性在血清尿酸水平超过345umol/l以后发生高血压的风险升高,尿酸水平每增加1mg/dl,其发生高血压的风险增加25%。
3.青年女性在血清尿酸水平超过214umol/l以后发生高血压的风险升高。
在2013年8月出版的《风湿病学年鉴》(Ann Rheum Dis)杂志上,发表了美国阿拉巴马州伯明翰大学风湿免疫系Angelo L Gaffo等人的一项队列研究结果。研究旨在分析血清尿酸水平是否与青年人的高血压发病存在相关性。【原文下载】
该回顾性队列分析来源于青年人冠状动脉危险因素(CARDIA)研究,共纳入了4752例基线状态时无高血压病的青年人的血清尿酸水平。该研究起始于1985年,为一项人种混合性(美国黑人和白人)队列研究,收集了20年的随访数据以供分析。基线状态时的血清尿酸水平与高血压病(血压≥140/90mmHg或使用降压药物)的相关性通过性别二项变量和多变量Cox比例分析进行评估。
研究开始时,男性青年人的平均年龄为24.8岁,女性为24.9岁。对比不同尿酸水平区间分组,研究者发现,男性青年人发生高血压的风险在其血清尿酸水平达到345umol/l(5.8mg/dl)以后逐渐升高,而女性的相应数值为214umol/l(3.6mg/dl)。男性青年人的血清尿酸水平每增加1mg/dl,其发生高血压的风险则增加25%,而对女性的研究则未发现类似相关性。
研究者认为,即使血清尿酸水平尚未达到404umol/l(6.8mg/dl)的低限参考值,但偏高的血清尿酸水平还是与高血压发病的潜在风险存在相关性。
研究背景:
对50岁以上成年人的研究发现,升高的血清尿酸水平与高血压发病之间存在明确相关性。对动物模型的研究发现,早期降尿酸治疗可以减少尿酸介导的高血压病的发生。一些小样本的流行病学研究发现,随着年龄增加,血清尿酸与高血压发病间的相关性逐渐降低,这可能源于年轻人对血清尿酸参与的高血压相关病变更加敏感。然而目前对成年人的随机临床研究仍主要集中于40岁以上人群,其动脉硬化已然形成,限制了降尿酸治疗对预防高血压形成的研究。
青年人冠状动脉危险因素(CARDIA)队列研究主要用于调查研究美国白种和黑种青年人发生的心血管疾病,该研究可用于评估青年人较高的血清尿酸水平与高血压发病之间的相关性。
原文下载
Gaffo AL, Jacobs DR Jr, Sijtsma F, Lewis CE, Mikuls TR, Saag KG.Serum urate association with hypertension in young adults: analysis from the Coronary Artery Risk Development in Young Adults cohort.Ann Rheum Dis. 2013 Aug;72(8):1321-7. doi: 10.1136/annrheumdis-2012-201916.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Dis#
47
#相关性#
34
#青年人#
37
#血清尿酸#
41