European Radiology:三维定量MRI技术可实现术前小肝癌的微血管浸润预测
2022-06-07 shaosai MedSci原创
钆剂增强磁共振成像(MRI)在检测HCC方面具有高度敏感性。文献报道表明,特定的MRI特征能够预测HCC中MVI的存在。
 肝细胞癌(HCC)是最常见的肿瘤之一,是全球癌症相关死亡的第三大原因。微血管侵犯(MVI)是导致HCC患者肿瘤复发,特别是早期复发的一个重要风险因素。在≤3厘米的小HCC中,MVI的发生率为18.1-37.0%。对于MVI阳性的小HCC患者来说,手术切除比射频消融(RFA)预后更佳。因此,探索在术前阶段识别MVI的方法十分重要。
肝细胞癌(HCC)是最常见的肿瘤之一,是全球癌症相关死亡的第三大原因。微血管侵犯(MVI)是导致HCC患者肿瘤复发,特别是早期复发的一个重要风险因素。在≤3厘米的小HCC中,MVI的发生率为18.1-37.0%。对于MVI阳性的小HCC患者来说,手术切除比射频消融(RFA)预后更佳。因此,探索在术前阶段识别MVI的方法十分重要。
钆剂增强磁共振成像(MRI)在检测HCC方面具有高度敏感性。文献报道表明,特定的MRI特征能够预测HCC中MVI的存在。然而,这些特征的能力是有限的。放射组学和深度学习是用于预测HCC中MVI的新兴方法,但其高通量数据的稳定性、建模方法和评价标准等方面的问题限制了应用。
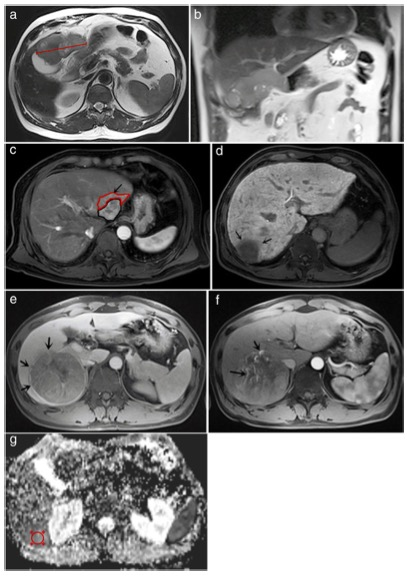
HCC的宏观分类与MVI有关。单一结节型伴结节外生长、多结节型和浸润型的复发率高于单一结节型。钆塞酸增强MR获得的高分辨率图像可以在宏观层面上对HCC进行分类。三维(3D)定量分析是一种对肿瘤特征提供更详细和可重复的定量评估技术。有报告指出,从肿瘤病变中提取的三维定量参数可用于术前诊断和风险分层。
近日,发表在European Radiology杂志的一项研究探讨了术前钆塞酸增强MR的三维定量分析和成像特征在MVI中的意义,以及预测因素与单个HCC≤3cm的术后早期复发之间的关系,为提高HCC患者的预后提供了影像学支持。
本研究回顾性地纳入了214名病理证实的HCC患者(训练队列:n = 169;验证队列:n = 45)。分析了三维定量参数(体积、球形度和压缩性)和常规MRI特征。使用单变量和多变量逻辑回归分析确定MVI的重要预测因素。根据预测模型构建了列线图,并使用Kaplan-Meier方法评估了重要预测因素和早期复发率之间的关系。
肿瘤呈球形(odds ratio [OR] = 0.000; p < 0.001)、肿瘤边缘不光滑(OR = 3.353; p = 0.015)和肝胆相期(HBP)的瘤周低信号(OR = 14.067; p = 0.003)是MVI的独立显著因素。当这三个因素相结合时,训练和验证队列的诊断特异性分别为97.0(128/132)和87.9(29/33)。基于预测模型的列线图在训练组(C-指数:0.885)和验证组(C-指数:0.869)表现令人满意。在训练(29.1% vs. 10.2%,p = 0.007)和验证(36.4% vs. 6.7%,p = 0.037)队列中,有两个或三个重要因素的患者的早期复发率明显高于没有的患者。
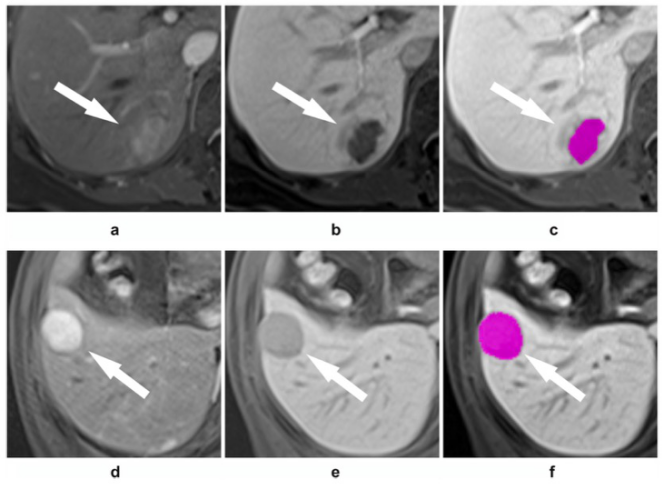
图 a-c 61岁女性,患有微血管浸润的肝细胞癌。a 钆塞酸增强MR的动脉期图像显示在肝脏第六段有一个2.8厘米的富血供肿块,并有瘤周强化。b 肝胆期图像显示为不光滑的肿瘤边缘和瘤周低信号。d-f 49岁男性,肝细胞癌,无微血管浸润。e 肝胆期图像显示肿瘤边缘光滑,没有瘤周低信号。肿瘤的球形度为0.818
总之,三维定量分析中较低的球形度、不光滑的肿瘤边缘和HBP上的瘤周低信号可以作为预测MVI的术前影像学指标,具有良好的预测性能,且与单个HCC≤3cm的手术后早期复发具有相关性。
原文出处:
San-Yuan Dong,Wen-Tao Wang,Xiao-Shan Chen,et al.Microvascular invasion of small hepatocellular carcinoma can be preoperatively predicted by the 3D quantification of MRI.DOI:10.1007/s00330-021-08495-4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#定量MRI#
51
#PE#
43
#小肝癌#
38
学习了
42
好文章,谢谢分享。
41
#微血管#
39