Spine:脊髓型颈椎病手术治疗功能预后的预测因素
2013-06-20 spine dxy
脊髓型颈椎病(CSM)是老年人最为常见的脊柱功能障碍。尽管大部分患者手术效果良好,但对这类疾病目前尚无很好的指标准确地预测患者术后的功能预后。有研究报道认为,MRI检查的相关影像学表现可以预测CSM的功能恢复情况,但因MRI测量方法学等的差异,目前并没有一个确定性的结论。同样的,大量的回顾性研究认为年龄,症状持续时间,改良JOA评分的基线水平等均和患者术后功能恢复相关。但近期的一项系统研究评价认为
脊髓型颈椎病(CSM)是老年人最为常见的脊柱功能障碍。尽管大部分患者手术效果良好,但对这类疾病目前尚无很好的指标准确地预测患者术后的功能预后。有研究报道认为,MRI检查的相关影像学表现可以预测CSM的功能恢复情况,但因MRI测量方法学等的差异,目前并没有一个确定性的结论。同样的,大量的回顾性研究认为年龄,症状持续时间,改良JOA评分的基线水平等均和患者术后功能恢复相关。但近期的一项系统研究评价认为,基于当前研究文献较多的局限性,如未对研究中各项混杂因素进行精确的控制等,针对CSM疾病预后推荐一个较为准确的预测指标较为困难14 注。日前来自加拿大的学者就CSM手术功能预后的相关预测因素进行了前瞻性研究,发现年龄和术前基线mJOA评分水平是预测CSM术后功能预后的两个较为可靠的指标,相关论文发表于近期的Spine杂志上。
研究数据来源于2006年2月至2007年11月间因CSM疾病在研究者所在医院行手术治疗的患者,期间共85例CSM手术,其中20例患者缺少MRI,4例患者失去随访而未纳入研究,共余61例患者,所有纳入研究患者均经MRI检查并结合临床症状,诊断为CSM,其中男42例,女19例,平均年龄57岁。
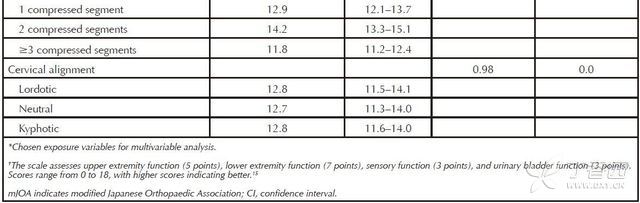
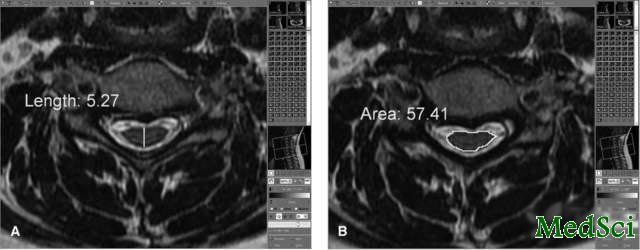
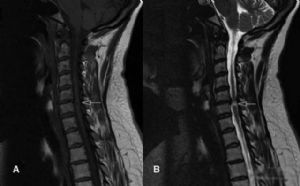
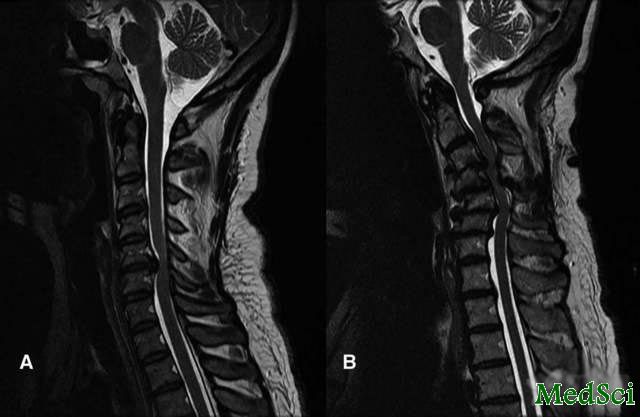
研究收集的数据包括:患者人口统计学数据;术前基线mJOA评分,术后12月mJOA评分;MRI影像学数据,如脊柱轴线,前后位直径(AP),最大压迫部位的横截面积(transverse area,TA,图1),脊髓信号强度(signal intensity,SI,图2),压迫节段(图3)。
图2:术前脊髓SI改变,T1低信号,T2高信号,信号改变分为三类:type 0, 正常T1WI/正常 T2WI;type 1,正常T1WI/高 T2WI, and type 2, 低T1WI/高 T2WI
研究结果如下
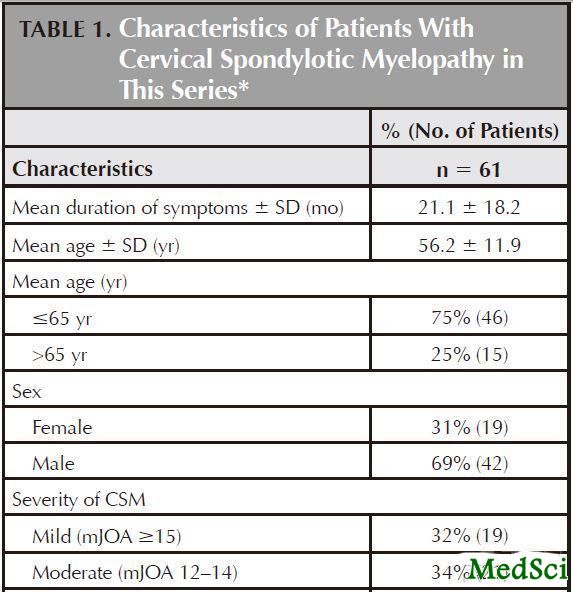
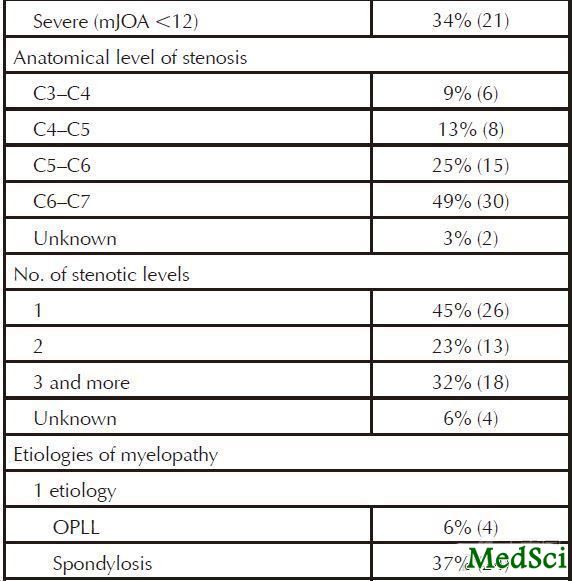
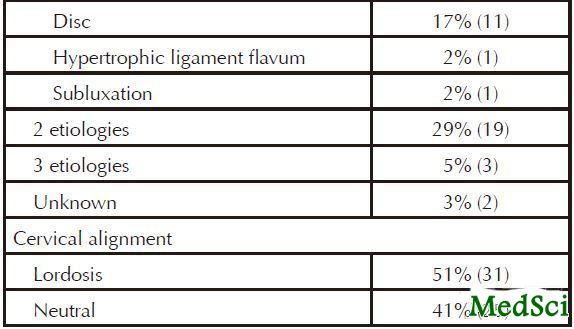
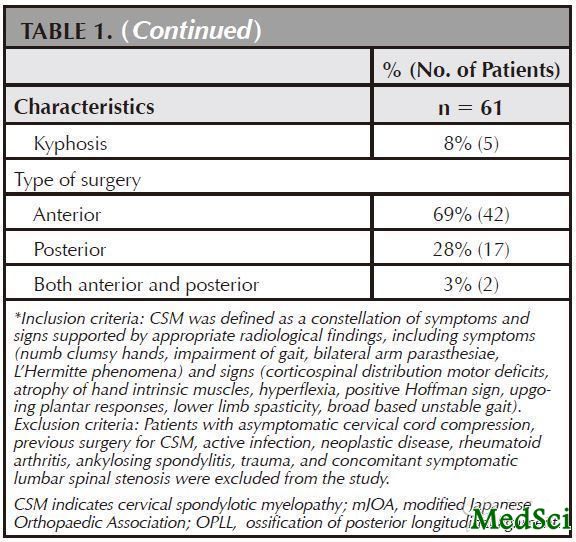
入选的患者人口统计学数据如表1所示。
表1:纳入研究的人口统计学数据
术后并发症发生率5%(3/65),2例声音嘶哑,术后6月得到恢复;1例脑脊液漏。术后12月只有5例患者出现神经功能恶化。手术1年内无患者死亡。
前路手术患者42例,后路手术17例,前后路联合2例。术后1年内无患者需要翻修。手术方式和mJOA评分无关(p=0.30)。平均mJOA评分术后较术前有显著改善(p<0.05)。
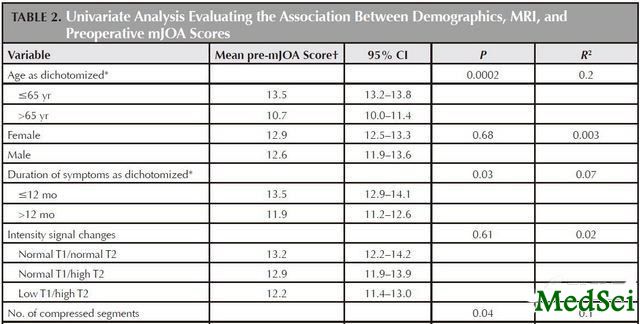
基线mJOA 水平和患者人口统计学及MRI 关系:年龄小于65岁组患者mJOA评分(13.5 ± 0.35)显著好于年龄大于65岁组(10.7 ± 0.72,p=0.0002);急性病程的患者(病史<12月)mJOA评分显著好于慢性病程患者(p=0.03);高基线水平的mJOA评分和较小的TA(r=0.28,p=0.02)相关;性别,SI改变,AP直径等和mJOA评分无关。如表2所示。
表2:基线mJOA水平和患者人口统计学及MRI关系多变量分析
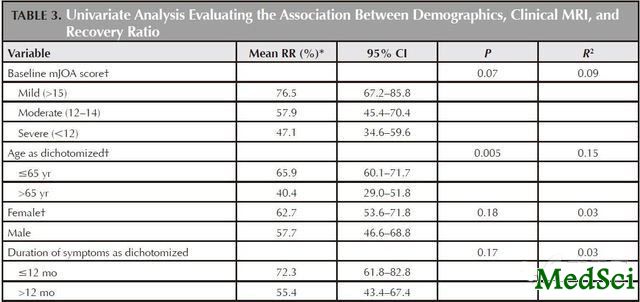
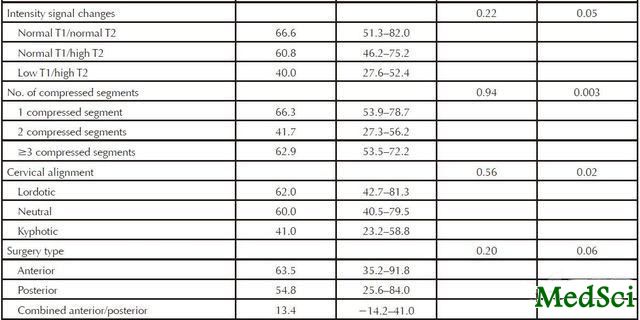
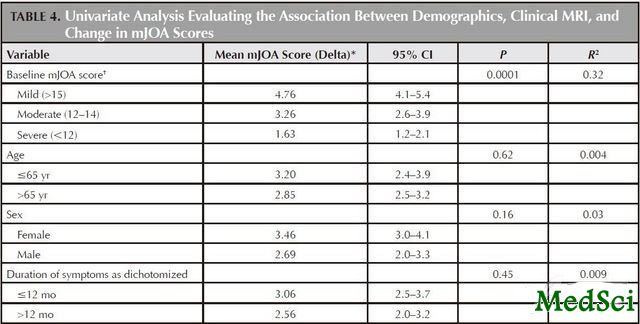
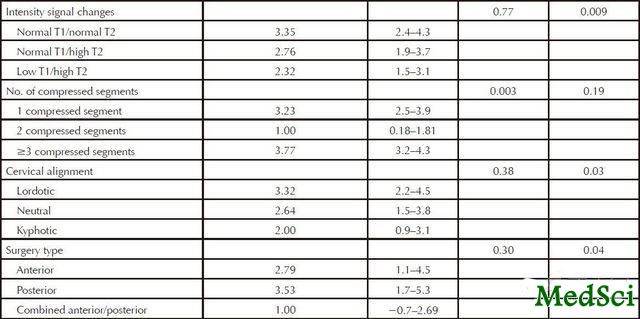
术后功能预后和患者人口统计学,临床症状,MRI 关系:年轻组恢复率65.9 ± 5.76%,老年组术后恢复率40.4 ± 11.42%,p=0.0053;急性病程组和慢性病程组恢复率分别为72.3 ± 10.47% 及12.4 ±0.72%;有较高基线水平mJOA患者恢复率好于较低基线水平患者(p=0.003),同时较高基线水平mJOA患者的评分改善率好于低基线水平患者(p=0.0001),如表3,4所示。
表3:恢复率和患者人口统计学,临床症状,MRI关系
表4:mJOA改善和患者人口统计学,临床症状,MRI关系
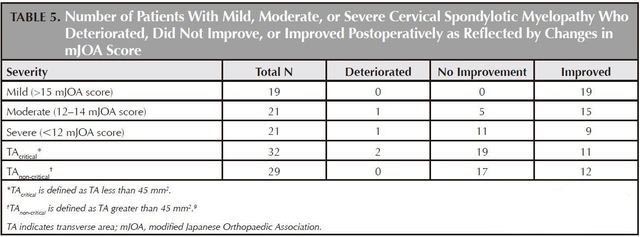
TA 和临床预后关系:定义TA临界值为45mm2,按TA临界值分组比较,未发现基线水平mJOA,恢复率,mJOA评分变化等组间差异(P = 0.17, P = 0.07,及P = 0.38),如表5所示。
表5:TA和临床预后关系
TA 和其他变量关系:高TA值和基线水平相关(r=0.29,p=0.02);年轻组患者的TA值显著大于年老组(r=-0.27,p=0.03);高脊髓T2信号改变患者TA值更小(r=-0.39,p=0.009)。
多因素方差分析:MRI相关变量不是衡量预后的一个可靠指标;年龄大于65岁患者基线水平mJOA评分较年龄小于65岁患者要小2.83倍;更高基线水平mJOA术后所可能获得更多的mJOA评分改善。
据上述研究结果,研究者在讨论中总结认为
1. 和CSM患者术后功能预后显著相关的两个强预测因子是年龄和基线mJOA评分:年龄小于65周岁和术后高mJOA评分改善相关;基线mJOA评分越高,术后获得mJOA分值改善越多。患者年纪较轻,mJOA评分越高提示脊髓神经病理变化越少,术后恢复的也越好。
2. 症状持续的时间和功能预后无显著相关性,但有相对趋势,即时间持续越久,功能预后倾向越差。该结论和其他使用JOA评分进行功能评估的临床研究相一致。
3. 按常理推测,在脊髓信号改变最强组脊髓压迫应当最小,即TA值最小;而无信号改变组TA值最大。研究中确实发现,无SI改变患者的TA值最高;但有趣的是,TA值最小组出现在单纯T2SI改变组,而非T1SI及T2SI改变组,提示我们T2相信号改变计较T1相可能对脊髓功能预后影响更大。TA和术前mJOA评分有显著相关性,但和术后功能预后无显著关系。一个可能的原因是:其他相关因素如年龄,基线mJOA水平等对最终结果影响太大而干扰了该项指标的显著性差异。
4. Fukeshima等人认为TA临界值为45mm2,而本研究中并未发现TA临界值分组患者在功能预后方面的差异,提示TA的临界值可能并不是45mm2.
据上,研究者认为:年龄和基线mJOA水平是CSM预后的重要预测因子;尽管脊髓压迫程度、患者术前症状持续时间两者和术前功能状态和年龄相关,但并不是功能预后的指标;脊髓SI改变并不是功能预后的预测因素。
[编者按]:对“脊髓SI信号改变不是功能预后的预测因素”存疑。对创伤性脊髓损伤的部分患者而言,脊髓信号改变可能是其唯一的影像学阳性检查结果,提示存在脊髓损伤,在临床上我们通常认为创伤患者的脊髓信号出现改变往往可能预示预后不佳。对非创伤的患者,脊髓信号改变的意义到底对功能预后有何意义,个人认为取决于脊髓信号改变的病因,脊髓信号变化的原因很多,神经损伤,单纯脱髓鞘变化等均可能出现脊髓信号改变,这两种改变对脊髓功能的影响是不一样的,百度或google搜索可以看到很多关于这方面的文章,各位战友可以看看。不当之处请各位战友指正。
注:本文有个角标14的,是文中列出的参考文献第14篇,如果需要查看具体的参考文献科目,可以下载原文查看。如果无法获得全文,各位战友可以PM联系我。

Predictors of surgical outcome in cervical spondylotic myelopathy.
STUDY DESIGN
Prospective study.
OBJECTIVE
To determine whether magnetic resonance imaging and clinical and demographic findings in patients with cervical spondylotic myelopathy (CSM) were independently associated with baseline functional scores and whether these were also predictive of postoperative functional outcomes.
SUMMARY OF BACKGROUND DATA
There are considerable limitations in current literature that prevent making formal recommendations regarding the use of clinical and radiological prognostic factors in patients with CSM.
METHODS
This prospective study included 65 consecutive patients with CSM treated in a tertiary referral center. The modified Japanese Orthopaedic Association (mJOA) scale was used to quantify disability at admission and at 12-month follow-up. Age, sex, duration of symptoms, severity of myelopathy, spinal column alignment, surgical technique, levels of compression, anteroposterior diameter and transverse area at the site of maximal cord compression, and magnetic resonance imaging signal intensity changes were assessed. Data were analyzed using Spearman rank correlation test, analysis of variance, Mann-Whitney U test, and stepwise multivariate regression.
RESULTS
Higher baseline mJOA scores were associated with younger age (P = 0.0002), shorter duration of symptoms (P = 0.03), and greater transverse area (P = 0.02). Better recovery ratio was associated with younger age (P = 0.005) and higher baseline mJOA score (P = 0.003). Greater changes in mJOA score were associated with higher baseline mJOA score (P < 0.0001). Using multivariate analysis, the functional outcomes after surgery were best predicted by baseline mJOA score and age of patient.
CONCLUSION
Age and baseline mJOA scores were highly predictive of outcome for patients undergoing surgical treatment of CSM. The degree of spinal cord compression and patterns of signal intensity changes on T1/T2 weighted images were not independently predictive of outcome, but it was found to correlate with the functional status at the time of presentation and age of the patient. The duration of symptoms correlated well with preoperative functional status but did not seem to affect the postoperative outcome.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Spine#
35
#预测因素#
38
#手术治疗#
35
#功能预后#
37
#脊髓型颈椎病#
54