Elife:袭荣文实验室发现干细胞-子细胞扩增环路介导了再生和肿瘤发生
2017-04-25 佚名 北京生命科学研究所
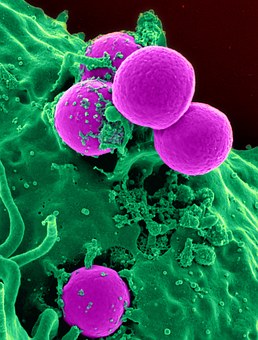
组织的再生能力与肿瘤的发生有密切的相关性,但其中的机制一直不能被解释。研究人员通过对果蝇肠上皮不同类型的细胞表达谱的比较,发现了一个在未分化细胞中特异表达的转录因子Sox21a. 用制备的抗体染色发现Sox21a 在将要分化的细胞中的表达有个明显的上调。通过CRISPR/Cas9基因组编辑技术,研究人员得到了Sox21a基因敲除果蝇,并惊奇地发现突变的果蝇在出生1-2周后即产生大量肠道肿瘤。进一步
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#eLife#
33
#Life#
38
学习了,感谢分享!
80
不明觉厉
78
学习了,谢谢作者分享!
80