J Clin Oncol:有无新辅助化学激素治疗的根治性前列腺切除术在局部和高风险前列腺癌中的疗效比较
2020-08-21 AlexYang MedSci原创
单独的根治性前列腺切除(RP)在治疗临床局部、高风险前列腺癌(PC)中往往是不够的。最近,有研究人员假设了在RP之前进行雄激素阻断治疗加多烯紫杉醇的化学激素治疗(CHT)能够改善生化无进展生存(BPF
单独的根治性前列腺切除(RP)在治疗临床局部、高风险前列腺癌(PC)中往往是不够的。最近,有研究人员假设了在RP之前进行雄激素阻断治疗加多烯紫杉醇的化学激素治疗(CHT)能够改善生化无进展生存(BPFS)。
研究总共包括了788名男性,并随机分配到RP组和新辅助CHT+RP组。随访时间均值为6.1年。研究发现,化疗期间,3级和4级副作用事件发生的总比例分别为26%和19%。研究人员在新辅助CHT+RP治疗和RP治疗之间没有发现3年BPFS存在差异(0.89 vs 0.84,95%CI:-0.01到0.11; P=0.11)。另外,与RP单独治疗相比,新辅助CHT与总的BPFS改善(HR,0.69;95%CI:0.48到0.99)、MFS的改善(HR, 0.70; 95% CI:0.51到0.95)和OS的改善(HR, 0.61; 95% CI:0.40到0.94)相关。
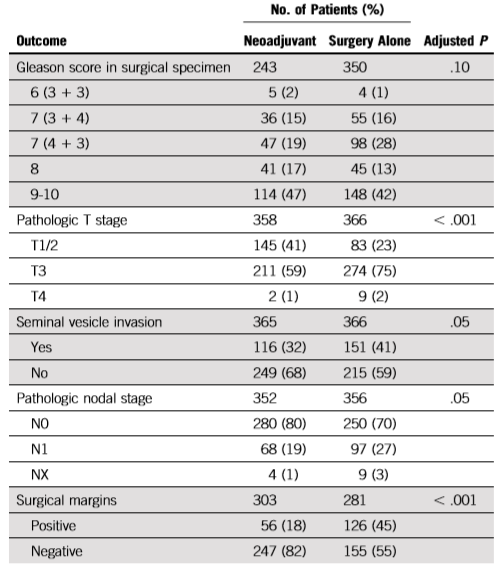
CHT+RP治疗或者单独RP治疗的病理结果
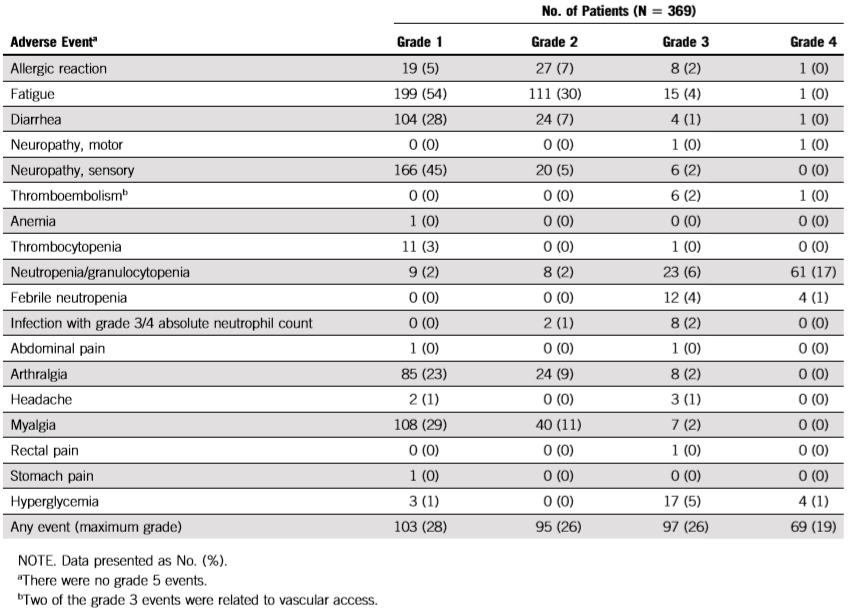
接受新辅助化学激素治疗的副作用事件
最后,研究人员指出,主要的研究结果终点和3年BPFS没有满足预期。尽管在次级终点中有所改善,但必须权衡益处和毒性。因此,他们的结果不支持在局部高风险PC患者中使用新辅助CHT+RP治疗。
原始出处:
James A Eastham, Glenn Heller, Susan Halabi et al. Cancer and Leukemia Group B 90203 (Alliance): Radical Prostatectomy With or Without Neoadjuvant Chemohormonal Therapy in Localized, High-Risk Prostate Cancer. J Clin Oncol. Jul 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
25
#高风险#
25
#新辅助#
22
#前列腺切除#
34
#切除术#
26
哦,这样啊
75
#激素治疗#
38
#局部#
23
#根治#
28
谢谢梅斯提供这么好的信息,学到很多
43