European Radiology:RCC超声引导下经皮MWA治疗,真的经得起时间的考验吗?
2021-11-22 shaosai MedSci原创
对于被诊断为临床T1a(cT1a)肾细胞癌(RCC)的患者,治疗的目标是在去除肿瘤的情况下尽可能大的保留正常肾实质的。

对于被诊断为临床T1a(cT1a)肾细胞癌(RCC)的患者,治疗的目标是在去除肿瘤的情况下尽可能大的保留正常肾实质的。现阶段,消融术是可保留肾实质的重要术式之一。然而,国际指南建议,消融术主要应用于肿瘤直径3厘米以下或无法进行手术的RCC患者。
微波消融(MWA)作为一种新兴的消融技术,具有温度高、消融量大、消融时间短等优势,已被广泛应用于多种肿瘤的治疗。在2005年首次应用于RCC治疗后,RCC的MWA在过去十年中取得了快速发展。与RFA和CA类似,RCC的MWA可以通过经皮、开放或腹腔镜方法进行。超声(US)和计算机断层扫描(CT)引导下的经皮通路是RCC的MWA中最常用的方法。
与CT相比,US的优点是实时、便宜、方便,而且没有辐射或肾脏毒性。然而据我们所知,对MWA在cT1 RCC中的表现及效果评估的相关研究十分有限。近日,发表在European Radiology杂志的一项研究为US引导下经皮MWA治疗cT1 RCC提供了实战经验,并为大众提供了成熟的随访和大型多中心累积数据,为US MWA的进一步广泛应用铺平了道路。
本项回顾性研究回顾了2006年4月至2019年12月期间接受微波消融手术的T1N0M0肾细胞癌患者,并收集了临床病理和程序数据。评估了技术效果和并发症,并采用Kaplan-Meier方法进行癌症特异性生存、无病生存、总生存和局部肿瘤过程分析。
共有323名连续患者(平均年龄,62.9岁±14.0),371个活检证实的肿瘤(平均直径,2.9厘米±1.2)入选,42.6%的肿瘤位于集合系统/肠道附近,360个(97.0%)肿瘤达到技术有效性。对于275名cT1a患者,在中位随访时间为66.0个月(IQR,58.4-73.6),10年的局部肿瘤进展、癌症特异性生存、无病生存和总生存率分别为1.9%、87.4%、71.8和67.5%。对于48名cT1b患者,在30.4个月的中位随访时间内(IQR,17.7-44.8),5年的局部肿瘤进展、癌症特异性生存、无病生存和总生存率分别为11.3%、91.4%、69.1和89.2%。主要并发症在cT1a(3.5%)和cT1b(6.9%)患者之间没有差异(p = 0.28)。基于多变量模型建立的临床风险分层系统可以预测DFS和CSS,其c指数分别为0.78(95%CI:0.71-0.85)和0.77(95%CI:0.65-0.90)。
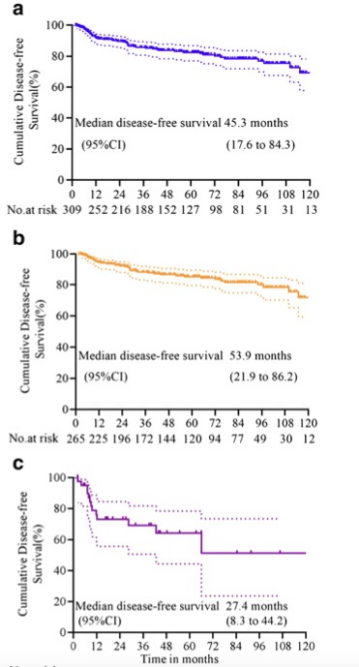
图 Kaplan-Meier分析疾病生存率。a 所有cT1患者。b cT1a组。cT1b组。竖线表示删减的病人。
本研究提供了超过10年的多机构经验,研究结果拥有全球最大的cT1 RCC的MWA队列,研究结果显示,MWA术后患者具有良好的生存预后和较低的肿瘤进展,为RCC患者提供了一个极佳的术式选择。
原文出处:
Jie Yu,Hui Wang,Zhi-Gang Cheng,et al.A multicenter 10-year oncologic outcome of ultrasound-guided percutaneous microwave ablation of clinical T1 renal cell carcinoma: will it stand the test of time?DOI:10.1007/s00330-021-07900-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#超声引导#
42
#超声引#
41
#PE#
27
#RCC#
48