Autoimmun Rev:系统性红斑狼疮妇女导致生育异常的相关因素
2022-01-14 从医路漫漫 MedSci原创
系统性红斑狼疮(SLE)是一种慢性自身免疫性疾病,主要影响育龄期成年女性。
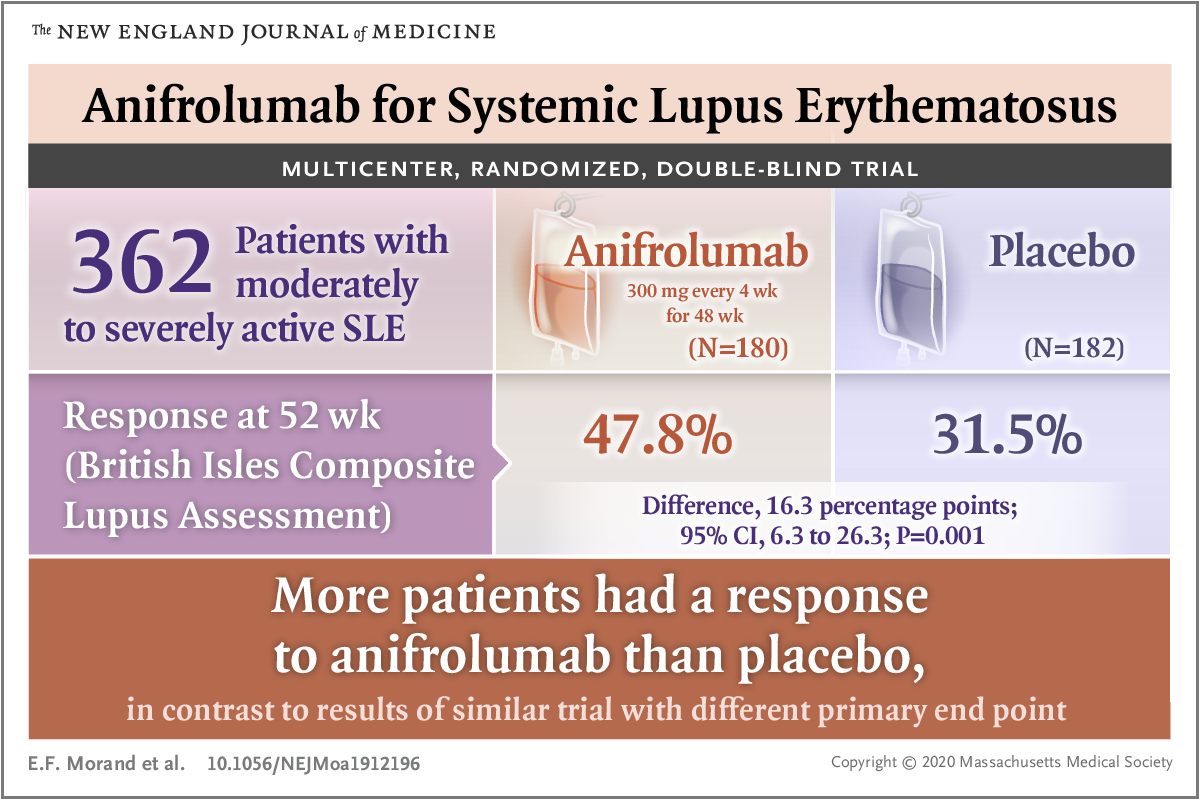
背景:系统性红斑狼疮(SLE)是一种慢性自身免疫性疾病,主要影响育龄期成年女性。在这些患者中,生育能力是一个值得关注的领域,因为与疾病相关的因素(例如更高的疾病活动,狼疮发作或疾病相关的损伤),慢性疾病的社会心理影响以及药物暴露可能会损害性腺功能。生育率是所有风湿病学家在SLE妇女管理中应考虑的一个重要方面,以便选择适当的治疗方法来保证和保护其生育能力。SLE卵巢功能衰竭的病理生理机制尚未完全确定,但可合理涉及外在因素(如治疗相关)和内在因素(如疾病相关)的共同影响。环磷酰胺(CYC)是一种免疫抑制药物,用于存在严重的主要器官受累,包括狼疮性肾炎和急性神经精神疾病(NP)。一些研究表明,SLE患者的环磷酰胺治疗与月经紊乱/闭经/卵巢早衰(POF)有关,与治疗时的累积剂量和患者年龄有关。在使用该治疗方法之前,应考虑使用促性腺激素释放激素类似物(GnRH-a)保留生育的能力。其他免疫抑制剂与生育异常的关系未知。目的:本系统文献综述(SLR)旨在探讨育龄期SLE妇女患者与生育结果相关的临床、激素、血清学和治疗因素。
方法:本SLR是按照系统评价和荟萃分析(PRISMA)的首选报告项目进行的。都经过Pubmed、EMBASE、Scopus和Cochrane图书馆的所有英文文章(1972 - 2021年4月30日)筛选。研究选择和数据收集由两名独立的审稿人完成。所有数据都是使用标准化模板提取的。使用NIH偏倚风险工具评估纳入研究的偏倚风险。
结果:在评估的789篇摘要中,我们纳入了46项研究,其中1项SLR研究、16项横断面研究、18项队列研究、10项观察性研究和1个病例系列研究,数据涉及4704例患者(平均年龄31.5±3.7岁,病程83.27±38.3个月)。研究中采用的卵巢早衰(POF)的定义因考虑闭经的月数和闭经的发病年龄而异。与POF发生相关的临床因素是开始治疗时年龄较大,以及SLE发病时年龄较大。19项研究报告称,环磷酰胺暴露(CYC)及其累积剂量影响SLE妇女的性腺功能,导致闭经和POF。与CYC相比,霉酚酸盐、硫唑嘌呤、钙调磷酸酶抑制剂和类固醇与POF相关的风险较低。与未接受GnRH-a治疗的患者相比,CYC和GnRH-a联合治疗的患者发生POF的频率较低(风险比0.798,95%-CI [0.1417;0.5525])。11项研究评估了损伤累积和疾病活动对卵巢储备的影响,但证据相矛盾。最后,18项研究调查了激素和血清学因素的暴露情况,其中Anti-Müllerian激素和黄体抗体都与POF无关。
结论:关于育龄SLE妇女生育相关因素的最强证据仍然是CYC治疗,以及其累积剂量。激素和血清学因素似乎不会影响生育结果,但它们可能用于评估生育状况,特别是在使用特定疾病的药物治疗期间。
原文出处:Giambalvo S, Garaffoni C, Silvagni E,et al.Factors associated with fertility abnormalities in women with systemic lupus erythematosus: a systematic review and meta-analysis.Autoimmun Rev 2022 Jan 04
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#系统性#
48
#狼疮#
35
#红斑#
43
#相关因素#
41
学习了#学习#
66