Lancet Respirat Med:Tezepelumab对中重度哮喘患者的气道炎性细胞、重塑、高反应性的影响
2021-07-12 MedSci原创 MedSci原创
Tezepelumab治疗可显著减少哮喘患者气道粘膜下的嗜酸性粒细胞
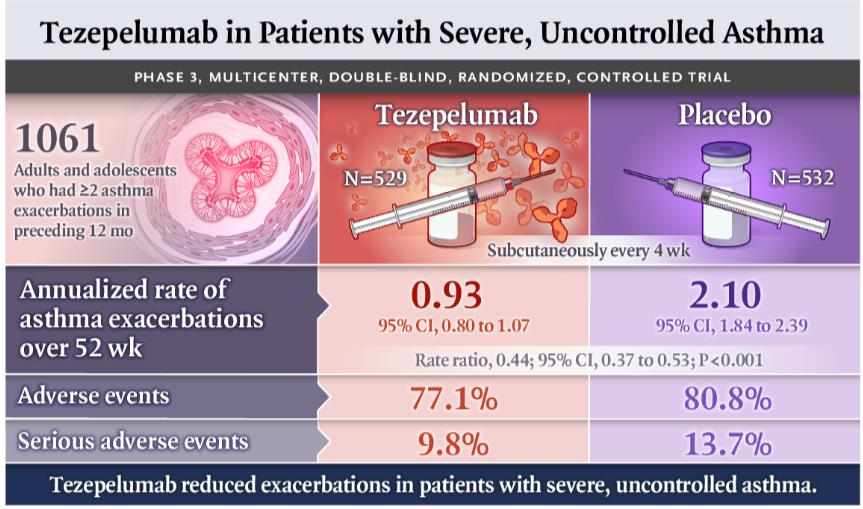
Tezepelumab是一种人单克隆抗体,可阻断胸腺基质淋巴细胞生成素(TSLP,一种上皮细胞来源的细胞因子)的活性。在2b期和3期试验中,Tezepelumab较安慰剂显著减轻了重度失控哮喘患者的恶化,且不受基础2型炎症生物标志物的限制。
本研究旨在通过Tezepelumab对气道炎性细胞、气道重塑和气道超敏反应的影响来研究Tezepelumab的作用机制。
CASCADE是一项在多个国家的27个医疗中心开展的探索性、双盲、随机化、安慰剂为对照的、平行组的2期研究,招募了18-75岁的失控的中重度哮喘患者,1:1随机分成两组,接受Tezepelumab(210 mg,1次/4周,计划28周)或安慰剂处理;如果因为新冠疫情影响了受试者治疗后的评估,随访则延长至52周。主要终点是支气管镜活检样本中气道黏膜下炎性细胞数量的变化。
2018年11月2日-2020年11月16日,共招募了250位患者,其中116位被随机分组:Tezepelumab组 59位,安慰剂组 57位。Tezepelumab组的48位患者和安慰剂组的51位患者完成了研究,被纳入主要终点评估。
两组嗜酸性粒细胞计数的变化
与安慰剂相比,Tezepelumab治疗可显著降低气道粘膜下的嗜酸性粒细胞(p<0.0010),该差异见于根据基线生物标志物划分的所有亚组。两个治疗组之间的其他评估的细胞(中性粒细胞、CD3+ T细胞、CD4+ T细胞、类胰蛋白酶+肥大细胞和糜酶+肥大细胞)则没有差异。
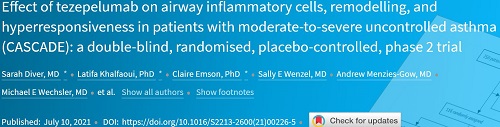
T2炎症生物标志物的变化
在次要终点评估中,两组的网状基底膜厚度和上皮完整性方面没有显著差异。在探索性分析中,与安慰剂相比,Tezepelumab可显著降低患者的甘露醇气道高反应性。最后,两组各有90%的患者报告了不良事件。
综上所述,在既往研究中所观察到的采用Tezepelumab治疗所带来的哮喘临床效益可能是,至少部分是,通过降低嗜酸性气道炎症实现的。Tezepelumab还可降低对甘露醇的气道高反应性,表明除了减少2型气道炎症外,TSLP阻断剂可能对哮喘具有额外的益处。
原始出处:
Sarah Diver, et al. Effect of tezepelumab on airway inflammatory cells, remodelling, and hyperresponsiveness in patients with moderate-to-severe uncontrolled asthma (CASCADE): a double-blind, randomised, placebo-controlled, phase 2 trial. The Lancet Respiratory Medicine. July 10, 2021. https://doi.org/10.1016/S2213-2600(21)00226-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PE#
31
#mAb#
35
#中重度哮喘#
48
#反应性#
38
#重度哮喘#
39
#Lancet#
33
#Tezepelumab#
44
#Med#
45
#PEL#
30
顶刊就是不一样,质量很高,内容精彩!学到很多
66