赛诺菲/再生元的Dupixent在第二次慢性自发性荨麻疹研究中表现欠佳
2022-02-18 Allan MedSci原创
赛诺菲和再生元制药本周五表示,基于预先指定的中期分析,Dupixent (dupilumab) 用于慢性自发性荨麻疹 (CSU) 患者的 III 期研究将因无效而停止。
赛诺菲和再生元制药本周五表示,基于预先指定的中期分析,Dupixent (dupilumab) 用于慢性自发性荨麻疹 (CSU) 患者的 III 期研究将因无效而停止。LIBERTY-CUPID B 试验旨在评估Dupixent (dupilumab) 在对罗氏和诺华的 Xolair(奥马珠单抗)耐药的患者中的有效性。
根据赛诺菲和再生元的说法,尽管在减少瘙痒和荨麻疹方面存在“积极的趋势”,但结果并未显示出对主要终点的意义。
去年,两家公司报告称,晚期 LIBERTY-CUPID A 试验证明,Dupixent (dupilumab) 在未接受过生物治疗的中度至重度 CSU 患者中实现了其主要和关键次要终点,将该药物添加到抗组胺药中显著降低了瘙痒和荨麻疹活动评分。Dupixent (dupilumab) 和安慰剂之间的总体治疗相关不良事件 (TEAE) 发生率相当:35 (50.0%)/40 (58.8%),注射部位反应发生率为 8 (11.4%)/9 (13.2%),严重 TEAE 为 2 (2.9%)/5 (7.4%)。
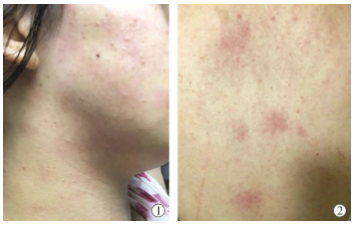
荨麻疹也称为风疹,是一种会引起瘙痒风疹的皮肤反应,风疹的大小从小斑点到大片不等。荨麻疹可由许多情况和物质引发,包括接触某些食物或药物。荨麻疹常在患者罹患感染症时,或是对于药物、蚊虫叮咬,或食物过敏后出现。心理压力、失温、或震动都有可能诱发。半数以上的荨麻疹病因都不明。避免接触过敏原是最重要的治疗方式。主要的治疗方式为使用苯海拉明、雷尼替丁等抗组织胺药。较为严重的案例可能会使用皮质类固醇或白三烯素剂。环境气温保持凉爽,也会有所帮助。

原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Dupixen#
49
#麻疹#
50
#Dupixent#
48
#慢性自发性荨麻疹#
63
#自发性#
41
受益匪浅
54
学习了
49
学习了,谢谢分享
53
学习了,谢谢分享
47