IBD:克罗恩病患者中一个遗传变异与手术后疾病复发密切相关
2021-11-21 MedSci原创 MedSci原创
克罗恩病:一种消化道的慢性、反复发作和非特异性的透壁性炎症, 病变呈节段性分布, 可累及消化道任何部位,其中以末端回肠最为常见,结肠和肛门病变也较多。
克罗恩病是一种会引起胃肠道任何部位的慢性炎症。有研究显示,在被确诊时,有40% 的患者有回结肠疾病,30%的患者有小肠疾病,30%的患者有结肠疾病。CD 的位置在整个临床过程中相对稳定,有 15% 的患者在诊断 10 年后可能会发生疾病位置的变化。然而,疾病行为会随着时间发生显着变化。在超过 10 年的病程中,很大一部分最初表现为非狭窄性、非穿透性 CD 表型的患者进展为狭窄性 (27%) 或穿透性 (29%) 疾病。CD 相关并发症的治疗通常需要手术干预,70%–80% 的患者在临床过程中需要某种手术治疗。此外,发现手术后3年内CD复发率为 30%。
早期研究表明CD相关易感性候选基因与狭窄回肠疾病与手术需要和NOD2基因变异之间存在关联。欧洲 IBDchip组织将NOD2基因确定为回肠艰难梭菌肠炎感染、回肠狭窄的主要影响遗传预测因子,至于NOD2在术后手术复发中的作用,最近的一项荟萃分析研究报告称,NOD2与手术复发无显着相关性(OR,1.58 [0.97–2.57];P = 0.06)。因此,遗传学对 CD 患者术后手术复发风险的作用仍有待阐明。本项研究旨在通过跨基因组的无假设搜索来确定临床和遗传风险因素模型,该模型可以预测 CD 患者首次腹部手术后的手术复发风险。
为了进行研究验证,两项独立的炎症性肠病 (IBD) 队列研究用于推导和验证遗传风险概况。使用 Illumina Immunochip 定制基因分型阵列对研究对象进行基因分型。手术复发定义为在第一次腹部手术后进行了第二次或多次腹腔肠切除术;非手术复发被定义为在第一次腹部手术后没有进一步的腹部切除术。

研究结果显示在研究入组时至少接受过1次腹部手术的372名CD患者中,132 名(35.5%)在第一次腹部手术后再次手术复发,240 名(64.5%)在随访结束时不需要进行后续腹部手术。在临床因素中,多变量分析显示免疫调节使用史( [OR],3.96;P=0.002)和CD首次手术较早(OR,1.12;P = 1.01E-04)是主要影响因素。基因型关联测试在TCF4的 chr18q21.2处鉴定了一个全基因组显着位点——rs2060886,与手术复发风险相关(OR,dom,4.10 [2.37–7.11];P = 4.58E-08)。
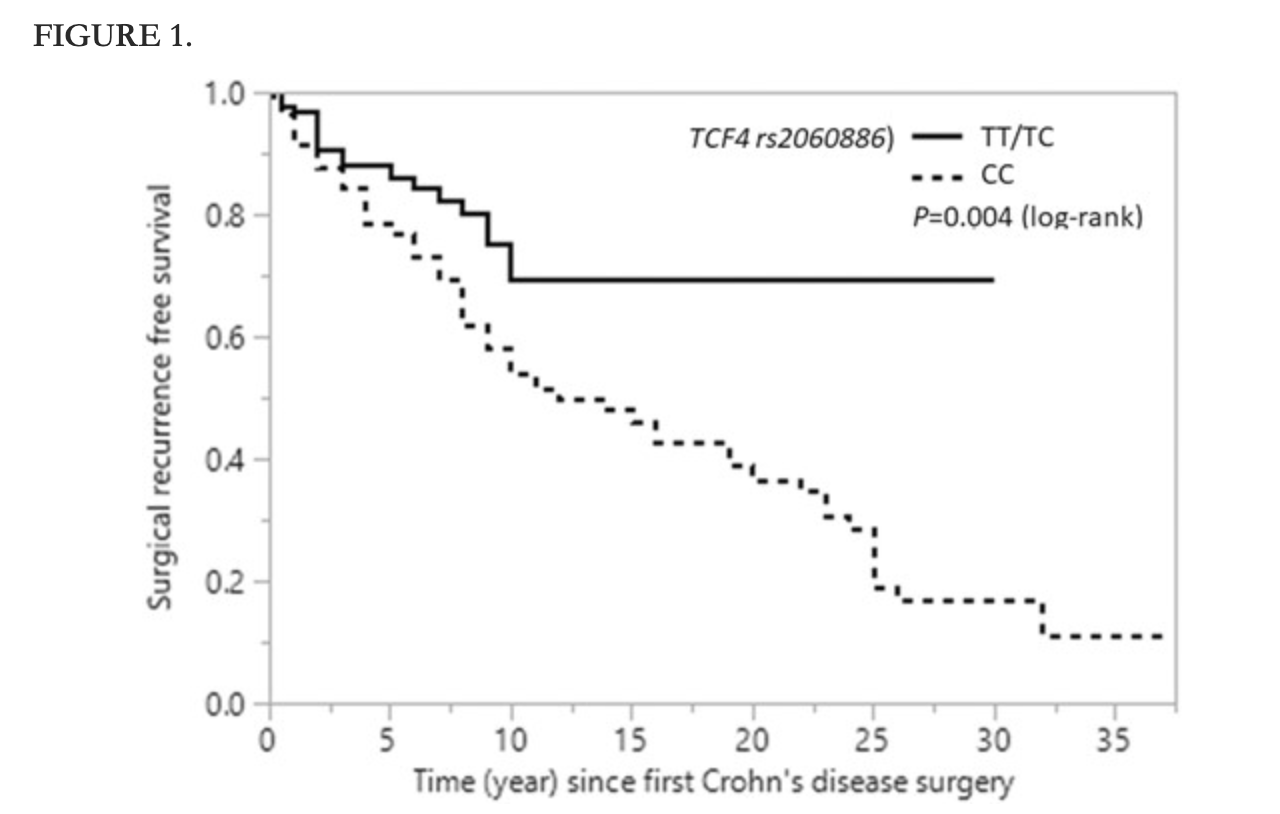
本项研究证实TCF4中的新的基因突变位点rs2060886与 CD 患者第一次腹部手术后全基因组显着性水平的手术复发风险相关。CD 首次肠道手术的时间与较高的手术复发风险相关。这些结果表明,遗传变异可能有助于指导重复腹部手术风险最高的患者的 CD 管理策略。
原始出处:
Ming-Hsi Wang. Et al. Novel Genetic Variant Predicts Surgical Recurrence Risk in Crohn’s Disease Patients. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疾病复发#
35
还行。。。。。
63
#IBD#
38
#变异#
46
#遗传变异#
45
学习了
72