Lancet Oncol:贝伐珠单抗或降低卵巢癌患者生活质量
2013-01-23 Lancet Oncol CMT
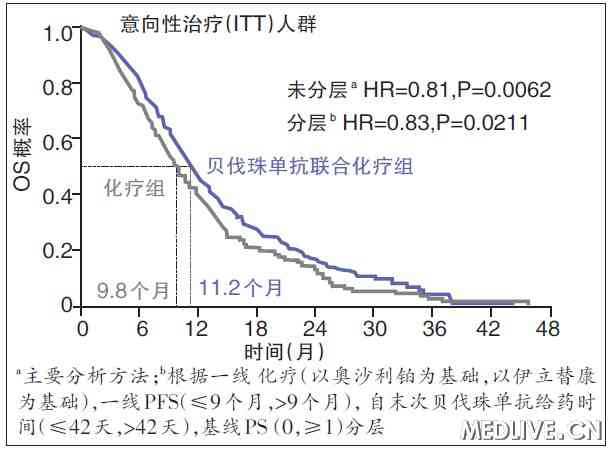
英法等国学者近期发表于《柳叶刀?肿瘤学》(Lancet Oncol)杂志的一项研究表明,对于卵巢癌术后患者,与单纯标准化疗相比,标准化疗联合贝伐珠单抗治疗可能与患者生活质量轻度但显著下降相关。在临床决策时应考虑权衡无进展生存期延长和生活质量下降。 在妇科肿瘤国际合作组卵巢肿瘤7(ICON7)临床试验中,贝伐珠单抗联合一线化疗并单独继续治疗18个周期可改善卵巢癌患者的无进展生存。
英法等国学者近期发表于《柳叶刀•肿瘤学》(Lancet Oncol)杂志的一项研究表明,对于卵巢癌术后患者,与单纯标准化疗相比,标准化疗联合贝伐珠单抗治疗可能与患者生活质量轻度但显著下降相关。在临床决策时应考虑权衡无进展生存期延长和生活质量下降。
在妇科肿瘤国际合作组卵巢肿瘤7(ICON7)临床试验中,贝伐珠单抗联合一线化疗并单独继续治疗18个周期可改善卵巢癌患者的无进展生存。对一个高危患者亚组进行的初步分析显示,总生存也有改善。该研究的目的是,描述ICON7临床试验中患者的健康相关生活质量(QOL)状况。
ICON7是一项随机、多中心、开放标签的Ⅲ期试验。2006年12月18日至2009年2月16日,已接受减瘤术的国际妇产科联盟(FIGO)分期Ⅰ~Ⅳ期高危卵巢上皮癌患者随机(1:1 )接受6个周期的标准化疗(卡铂AUC 5或6,紫杉醇175 mg/m2,共18周)或联合贝伐珠单抗(7.5 mg/kg)静脉注射,化疗结束后贝伐珠单抗继续应用(共54周)。
结果显示,764名女性被随机分配到标准化疗组,764例被分配到贝伐珠单抗组。基线时,标准化疗组684(90%)名女性和贝伐珠单抗组691(90%)名女性完成了生活质量问卷调查。54周时,502(66%)名贝伐单抗组女性和388(51%)名标准化疗组女性提交了生活质量数据。主要QOL终点采用欧洲癌症研究和治疗组织QOL问卷进行评估。
18周时所有女性的平均总QOL评分比基线时提高7.2分。54周时,标准化疗组的平均总QOL评分高于贝伐珠单抗组(76.1分 对 69.7 分,差异6.4分,P<0.0001)。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
31
#贝伐珠#
27
#Oncol#
27
#贝伐#
36