Stroke:Takayasu动脉炎患者的脑血管缺血事件
2022-04-03 MedSci原创 MedSci原创
颈动脉卒中/TIA在TA患者中较为常见。研究人员确定了TA患者脑血管缺血事件相关的因素。
Takayasu动脉炎(TA)是免疫介导的血管炎,其特征是大动脉肉芽肿性炎症。TA是一种可能并发脑血管缺血事件的大血管炎。

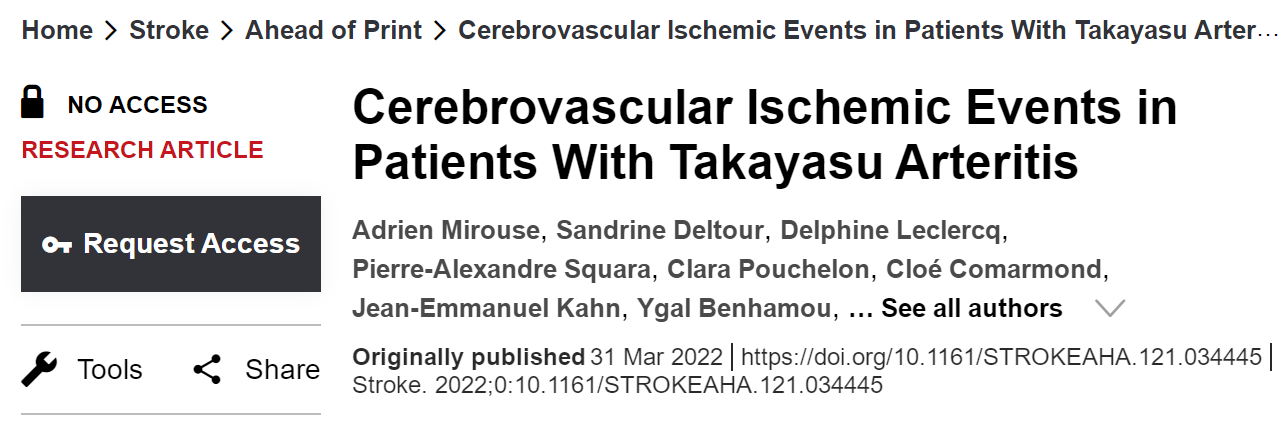
近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,该研究旨在描述伴有脑血管缺血事件TA患者的临床和血管特征,并确定这些事件的危险因素。
研究人员在一个大队列中分析了卒中/短暂性脑缺血发作(TIA)的患病率和类型,与脑血管缺血事件相关的因素,以及符合美国风湿病学会或Ishikawa的TA标准的无卒中生存期。
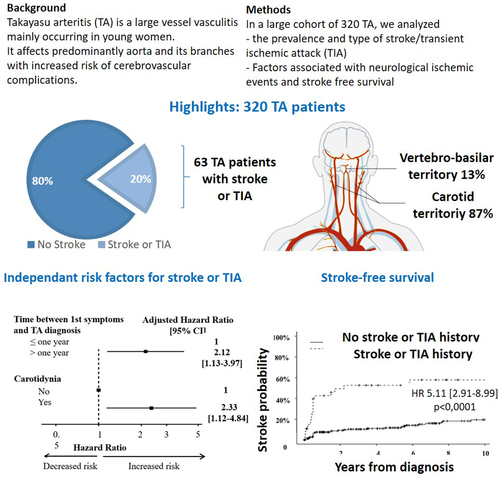
320例TA患者(诊断时中位年龄为36[25-47]岁;261例(86%),63例(20%)有卒中(n=41;65%)或TIA (n=22;35%)。缺血性事件集中在颈动脉的患者有55例(87%),椎动脉区8例(13%)。33例(52%)患者伴有多发狭窄,狭窄数量中位数2处(最少0处~最多11处),10例(16%)患者伴有动脉瘤。TA诊断前卒中或TIA病史(风险比[HR]为 4.50 [2.45-8.17];P<0.0001)、吸烟(HR为1.75 [1.01-3.02];P=0.05)、心肌梗死史(HR为0.21 [0.05 - 0.89];P=0.039)、胸主动脉受累(HR为2.05 [1.30-3.75];P=0.023)、从首次出现症状到诊断的时间>1年(HR为2.22 [1.30-3.80];P=0.005)和阿司匹林治疗(HR为1.82 [1.04-3.19];P=0.035)与脑血管缺血事件相关。在多因素分析中,从首发症状到TA诊断的时间>1年(HR为2.16 [1.27-3.70];P=0.007)与TA患者的脑血管缺血事件独立相关。相比于无卒中/TIA的患者,卒中/TIA患者脑血管缺血事件的HR为5.11 (2.91-8.99;P<0.0001)。
由此可见,颈动脉卒中/TIA在TA患者中较为常见。研究人员确定了TA患者脑血管缺血事件相关的因素。
原始出处:
Adrien Mirouse.et al.Cerebrovascular Ischemic Events in Patients With Takayasu Arteritis.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.034445
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉炎#
0
#Takayasu动脉炎#
63
学习了
47