Neural Regen Res:修饰脂质体可跨越血脊髓屏障及血脑屏障
2013-01-14 Neural Regen Res EurekAlert!中文
研究表明,单纯脂质体通过静脉注射后,仅有少量可以穿过血脑屏障。跨膜肽修饰的脂质体可以携带药物治疗颅内感染,同时经聚乙二醇修饰增加了其稳定性,并可以更长时间的存在于体循环中。一项关于“Transactivating-transduction protein-polyethylene glycol modified liposomes traverse the blood-spinal cord an
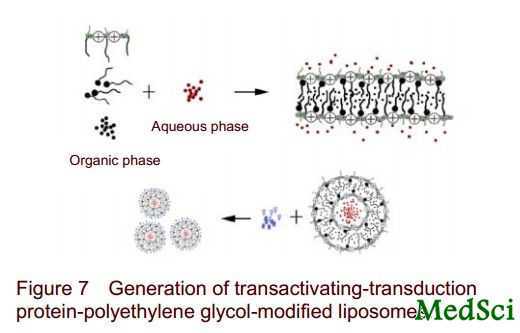
研究表明,单纯脂质体通过静脉注射后,仅有少量可以穿过血脑屏障。跨膜肽修饰的脂质体可以携带药物治疗颅内感染,同时经聚乙二醇修饰增加了其稳定性,并可以更长时间的存在于体循环中。一项关于“Transactivating-transduction protein-polyethylene glycol modified liposomes traverse the blood-spinal cord and blood-brain barriers”的研究以此制备跨膜肽、聚乙二醇修饰的脂质体,并以异硫氰酸荧光素荧光标记,使其同时兼备跨膜、长循环及荧光示踪特性,与人乳腺癌细胞进行共培养,观察其细胞摄取能力及细胞毒性作用,并通过大鼠静脉注射观察其跨越血脊髓屏障及血脑屏障的能力。研究显示,异硫氰酸荧光素修饰的跨膜肽-聚乙二醇-脂质体具有跨越大鼠血脊髓屏障及血脑屏障的能力,未来可将其携药治疗颅内感染等相关疾病,相关研究成果发表在《中国神经再生研究(英文版)》杂志于2012年12月35期出版的杂志上。

doi:10.3969/j.issn.1673-5374.2012.35.006
PMC:
PMID:
Xianhu Zhou1, Chunyuan Wang1, Shiqing Feng1, Jin Chang2, Xiaohong Kong3, Yang Liu1, Shijie Gao1
Naive liposomes can cross the blood-brain barrier and blood-spinal cord barrier in small amounts. Liposomes modified by a transactivating-transduction protein can deliver antibiotics for the treatment of acute bacterial infection-induced brain inflammation. Liposomes conjugated with polyethylene glycol have the capability of long-term circulation. In this study we prepared transactivating-transduction protein-polyethylene glycol-modified liposomes labeled with fluorescein isothiocyanate. Thus, liposomes were characterized by transmembrane, long-term circulation and fluorescence tracing. Uptake, cytotoxicity, and the ability of traversing blood-spinal cord and blood-brain barriers were observed following coculture with human breast adenocarcinoma cells (MCF-7). Results demonstrated that the liposomes had good biocompatibility, and low cytotoxicity when cocultured with human breast adenocarcinoma cells. Liposomes could traverse cell membranes and entered the central nervous system and neurocytes through the blood-spinal cord and blood-brain barriers of rats via the systemic circulation. These results verified that fluorescein isothiocyanate-modified transactivating-transduction protein-polyethylene glycol liposomes have the ability to traverse the blood-spinal cord and blood-brain barriers.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#脂质体#
27
#血脑屏障#
22
#修饰#
36