Sci Transl Med:第三军医大学罗阳团队利用AI在30秒内鉴定血型
2017-03-17 王新凯 奇点网
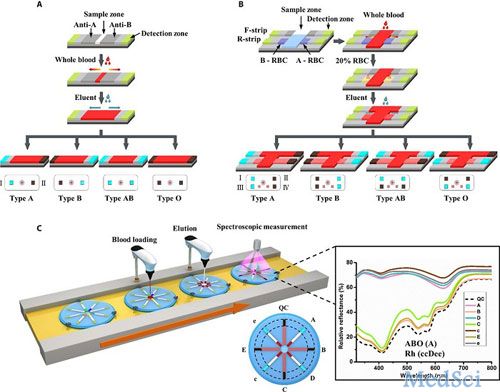
奇点原创3月15日,《Science Translational Medicine》期刊以封面的形式全文刊登了第三军医大学罗阳团队的研究成果!在很多人看来,查血型,只是一件“15块钱和半个小时”的小事情。而对于需要紧急输血的患者来说,能否及时得到所需的血源,关系到生死。就算是医院有足够的血源库存,输血前还要先花10-20分钟去鉴定血型,就有点耽误事情了。而且一旦发生配对失误,则会导致患者的免疫系统

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
33
#军医#
36
#Transl#
26
#Med#
27
非常好的研究
68