JAHA:肠道微生物的代谢物能增加不良心血管事件的风险?
2017-06-30 MedSci MedSci原创
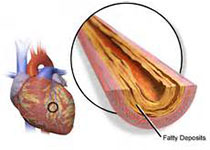
肠道微生物代谢物被认为是新型的心血管事件的危险因素,其中三甲胺-N-氧化物(TMAO)及其前体在血中的浓度与主要不良心血管事件(MACE)的关系尚未阐明。近日,在国际心血管权威杂志JAHA上发表了一篇旨在研究TMAO及其前体的血浓度与MACE之间关系的荟萃分析研究。
肠道微生物代谢物被认为是新型的心血管事件的危险因素,其中三甲胺-N-氧化物(TMAO)及其前体在血中的浓度与主要不良心血管事件(MACE)的关系尚未阐明。近日,在国际心血管权威杂志JAHA上发表了一篇旨在研究TMAO及其前体的血浓度与MACE之间关系的荟萃分析研究。 通过对PubMed和Embase数据库的搜索,本研究的主要分析共纳入了16篇文献中的19个前瞻性研究(n=19256,包括3315个事件),并使用多变量调整后的相对风险(RR)进行评估。研究结果表明相比于低浓度的TMAO,高血浓度的TMAO与MACE的复合RR相关(RR=1.62,95% CI 1.45—1.80,p=0.2,I2=23.5%),并且在一个临床研究中,黑色人种影响了这种相关性。排除了黑人数据后,RR在基于体重指数、糖尿病患病率、心血管疾病史和肾功能不全上无明显差异。此外,高浓度的TMAO与全因死亡率呈相关(RR=1.63,95% CI 1.36-1.95),拥有高浓度的TMAO前体(左旋肉碱,胆碱或甜菜碱)的患者的不良心血管事件的风险要比低浓度的高1.3-1.4倍。 本荟萃分析表明高血浓度的TMAO及其前体
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#微生物#
25
#代谢物#
31
#血管事件#
27
肠道微生物。
0
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
55
#AHA#
38
感谢分享!继续关注!
61