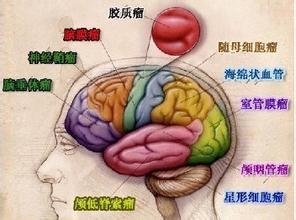
盘点:神经胶质瘤近期重要研究进展一览
2017-09-30 MedSci MedSci原创
神经胶质瘤系浸润性生长物,它和正常脑组织没有明显界限,难以完全切除,对放疗化疗不甚敏感,非常容易复发,手术难以切除或根本不能手术。化学药物和一般抗肿瘤的中药,因血脑屏障等因素的影响,疗效也不理想,因此神经胶质瘤至今仍是全身肿瘤中预后最差的肿瘤之一。这里梅斯小编整理了近期关于神经胶质瘤的重要研究进展与大家一同分享。【1】光学相干断层扫描可作为视神经胶质瘤儿童视力标志物马尼亚的Iuliu Hatieg
神经胶质瘤系浸润性生长物,它和正常脑组织没有明显界限,难以完全切除,对放疗化疗不甚敏感,非常容易复发,手术难以切除或根本不能手术。化学药物和一般抗肿瘤的中药,因血脑屏障等因素的影响,疗效也不理想,因此神经胶质瘤至今仍是全身肿瘤中预后最差的肿瘤之一。这里梅斯小编整理了近期关于神经胶质瘤的重要研究进展与大家一同分享。
【1】光学相干断层扫描可作为视神经胶质瘤儿童视力标志物
马尼亚的Iuliu Hatieganu医学与药学院眼科Banc A近日发表了一篇综述,系统阐述了光学相干断层扫描技术可作为视神经胶质瘤儿童一个视力标志物,来替代患病儿童的视力功能检查。对PubMed,Embase和Web of Science数据库进行搜索,纳入2000年至2016年间以英文发表的文章,同时要至少有10位参与者参加。结果共有11项研究符合标准,分析发现,视网膜光学相干断层扫描(OCT)是一种有潜力的工具,可以对患有视神经胶质瘤(OPG)儿童进行筛查或随访测试。同时,他们也提出需要进一步的多中心研究来支持。这项研究为临床眼科医生对治疗儿科视神经胶质瘤(OPG)提供了新的思路。
【2】中性粒细胞与淋巴细胞比值预测神经胶质瘤患者生存情况
神经胶质瘤,是发生于神经外胚层的肿瘤。大多缓慢发病,自出现症状至就诊时间一般为数周至数月,少数可达数年。研究人员收集了PubMed,EMBASE,Cochrane Library和NCBI中的相关文献,评估中性粒细胞与淋巴细胞比值(NLR)在神经胶质瘤患者中的预后作用。研究显示,升高的NLR与神经胶质瘤患者的总生存期较差有关。
【3】血糖和神经胶质瘤的发生也存在关联
神经胶质瘤是一种异质性原发性脑肿瘤,目前没有可以长期存活的治疗方法。诊断为胶质母细胞瘤的患者平均生存期14个月。症状通常仅在诊断前三个月才发生;因此,重要的是在症状发作前确定临床前肿瘤的指标。虽然糖尿病似乎增加了大多数恶性肿瘤的风险,在以前的16项研究中有11项都发现糖尿病与神经胶质瘤或所有类型的脑肿瘤之间存在逆关联。最近的荟萃分析证实了这种反向关系。
【4】弥漫性内皮神经胶质瘤全新治疗靶点
弥漫性内皮神经胶质瘤(DIPG)是一种高度危险的儿科脑干肿瘤,其特征是快速和渐进性导致患者死亡。在超过80%的这类肿瘤中组蛋白H3的杂合位点发生突变,并导致赖氨酸-甲硫氨酸置换(H3K27M)。这种组蛋白突变体的表达伴随着多梳抑制复合物(PRC2)介导的H3K27三甲基化(H3K27me3)水平的降低,这被认为是DIPG肿瘤发生的促进原因。研究人员使用DIPG的小鼠模型和原发性患者来源的DIPG细胞系,结果显示残留的PRC2活性是表达H3K27M的DIPG的增殖所需要的,并且EZH2是用于治疗这些肿瘤的潜在治疗靶点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









henhao
95
学习了谢谢分享
69
#神经胶质瘤#
43
#研究进展#
28
已学习.值得分享!
84
已学习.值得分享!
77