Alzheimer&Dementia:外周血CRP水平越低,老年痴呆风险越高!
2022-02-06 MedSci原创 MedSci原创
基线的低血浆CRP水平与普通人群中的AD高风险有关。
阿尔茨海默病(AD)和其他痴呆是常见的神经退行性疾病,影响超过4700万人。由于预期寿命的延长,估计到2050年,痴呆人数将增加3倍。目前针对痴呆尚无治愈性的治疗方案,而且大部分的基础生物学知识是未知的。有趣的是,最近有几项发现将AD和炎症联系起来——中年时血浆中C反应蛋白(CRP)水平的增加与AD风险的增加有关。
CRP是一种众所周知的急性期反应物,主要在肝脏中产生,已知其功能是激活补体系统,并通过Fcγ受体I和II(FCγRI和FCγRII)调节白细胞的行动。血脑屏障(BBB)完好的人的脑脊液(CSF)中的CRP水平与血浆中的CRP水平高度相关,因此血浆中的CRP水平可能反应了脑部CRP水平。CRP在AD患者大脑的神经纤维缠结和淀粉样斑块中被观察到,在大脑中局部产生,并且在AD大脑的受影响区域的mRNA和蛋白水平上调。

基于此,来自丹麦哥本哈根大学医院临床生物化学部的专家提出了低血浆CRP水平与AD和全因性痴呆风险增加有关的假设,并进一步测试了与低CRP水平相关的CRP的遗传变异是否与痴呆症的风险有关,相关结果发表在Alzheimer&Dementia杂志上。
为此,来自哥本哈根普通人群研究(CGPS)和哥本哈根城市心脏研究(CCHS)的111242人被纳入该研究,所有这些人都有基线血浆CRP测量。同时,测定了CRP基因的四个调节性遗传变体104,672人对rs3093077、rs1205、rs1130864和rs3091244。
结果显示,CRP百分位数组1-5(最低血浆CRP)与50-75组(参考)相比,AD的危险增加69%(HR=1.69,95%CI:1.29-2.16)。在体重指数≤25 kg/m2的个体中,遗传性低CRP与AD的风险增加有关(P = 4 × 10-6)。
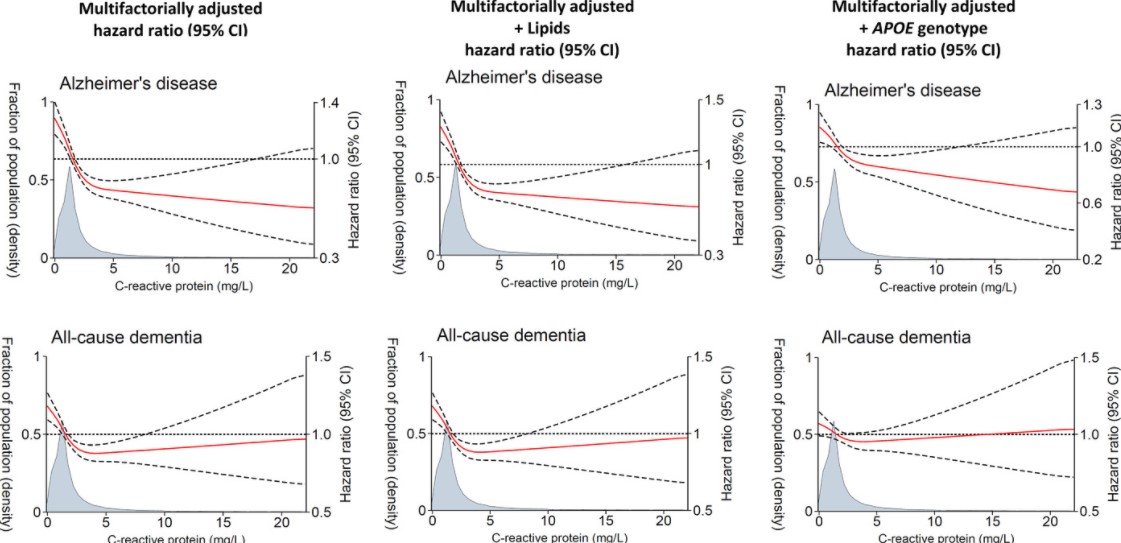
血浆CRP浓度与AD和全因性痴呆风险的关系
进一步将所有遗传分析按BMI≤25 kg/m2和BMI>25 kg/m2分层。CRP水平随着加权/简单等位基因得分组的逐步增加而下降。在BMI≤25 kg/m2的个体中,遗传性低CRP与AD的风险增加有关(趋势P=4×10-6)。加权/简单等位基因评分组5(最低CRP)与1(参考)相比,AD的HR=1.93(1.50-2.48),全因痴呆HR=1.43(1.18-1.73)。
综上,基线的低血浆CRP水平与普通人群中的AD高风险有关。这些观察性发现得到了遗传学研究的支持。
参考文献:
C-reactive protein levels and risk of dementia—Observational and genetic studies of 111,242 individuals from the general population. https://doi.org/10.1002/alz.12568
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#CRP水平#
49
#dementia#
37
新发现,新知识
70
#CRP#
51
#痴呆风险#
43
#外周血#
49
#学习#
57
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
22