Front Aging Neurosci:模拟运动或可改善阿尔兹海默氏症患者的病情
2016-04-07 佚名 生物谷
据美国阿尔兹海默氏症协会数据显示,阿尔兹海默氏症是引发美国人死亡的第六大原因,目前并没有有效的疗法和途径来减缓或抑制患者的病情进展,但患者可以通过机体和认知康复来获益,而且研究者目前也正在研究是否模仿行为可以作为一种有效工具来帮助重拾患者失去的能力。 近日,一项刊登于国际杂志Frontiers in Aging Neuroscience上的研究论文中,来自热那亚大学(University of
据美国阿尔兹海默氏症协会数据显示,阿尔兹海默氏症是引发美国人死亡的第六大原因,目前并没有有效的疗法和途径来减缓或抑制患者的病情进展,但患者可以通过机体和认知康复来获益,而且研究者目前也正在研究是否模仿行为可以作为一种有效工具来帮助重拾患者失去的能力。
近日,一项刊登于国际杂志Frontiers in Aging Neuroscience上的研究论文中,来自热那亚大学(University of Genoa)的研究人员通过研究发现,进行动作模仿或可帮助减缓阿尔兹海默氏症患者的症状;研究者指出,患者可以模拟人类简单的姿势或者电脑屏幕上移动的点,而这样的运动方式或许可以补充当前阿尔兹海默氏症的治疗策略。
重复别人的行为是一种基本的社会构建模块,其可以帮助人们去学习并且同他人交际,研究者Bisio指出,通过复制母亲的行为活动,婴儿就可以学会如何与人联系,而相同的原则也在网球学生中可以体现出来,网球学生可以向训练者学习如何进行网球的接发,相关研究结果就表明,模仿行为或许也可以用于帮助阿尔兹海默氏症患者进行疾病恢复。
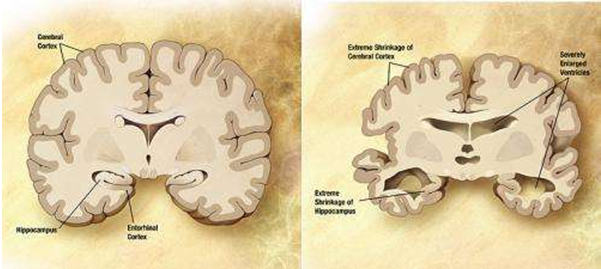
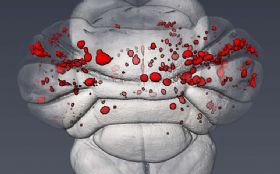
研究初期,科学家们并不确定是否具有多种连线的大脑功能在疾病刚开始造成损伤的时候就发挥作用,实际上阿尔兹海默氏症会以一种特殊的方式来毁灭大脑的某些功能,而本文研究中研究者发现,患者处于轻度疾病状态时可以保持自身的模仿能力,同时患者还可以很好地完成其训练者交给的模仿任务。
而基于电脑的训练方法可以为患者提供另外一种治疗方法,据研究者介绍,利用电脑进行训练是可能的,但以训练者为基础的训练方式或许更加有用,而这或许是因为患者在与训练者在接触交流过程中所产生的情绪反应所带来的益处要优于电脑的模拟训练。
最后研究者说道,由于阿尔兹海默氏症损坏了大脑中连接运动和认知功能的部分,而行为疗法对于患者而言非常重要,甚至在药物疗法后依然如此;通过让阿尔兹海默氏症患者模拟某些简单的行为活动获为后期开发更好的策略来改善或治疗阿尔兹海默氏症提供新的线索和希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#病情#
26
高大上的文章
110
d值得学习
124
#ROS#
24
#阿尔兹海默#
31