Metabolism:三羧酸循环相关代谢物与房颤和心衰风险的关系
2021-10-20 MedSci原创 MedSci原创
三羧酸(TCA)循环异常可能易患心血管疾病,这些结果突出了TCA循环在心脏结局发病机制中的潜在作用。
三羧酸(TCA)循环异常可能易患心血管疾病,但TCA循环相关代谢物在心房颤动(AF)和心力衰竭(HF)发生发展中的作用仍有待探索。

近日,代谢性疾病领域权威杂志Metabolism-Clinical and Experimental上发表了一篇研究文章,该研究旨在调查TCA循环相关代谢物与AF和HF风险之间的关联。
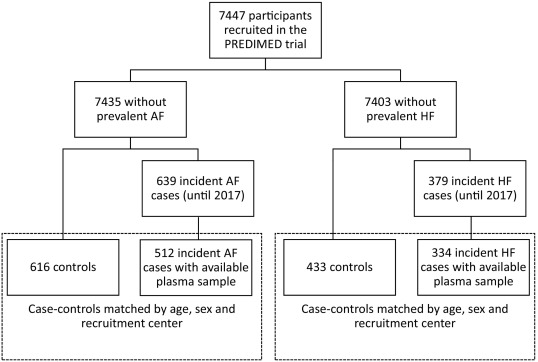
研究人员在PREDIMED研究中使用了两个嵌套病例对照研究。在大约10年的平均随访期间,该研究纳入了512名AF和334名HF病例,这些病例分别按年龄(±5岁)、性别和招募中心与616名对照者和433名对照者相匹配。研究人员使用液相色谱-串联质谱法测量了受试者血液中柠檬酸盐、乌头酸盐、异柠檬酸盐、琥珀酸盐、苹果酸盐和D/L-2-羟基戊二酸盐水平。研究人员采用拟合多变量条件Logistic回归模型以估计代谢物的比值比(OR)和95%置信区间(95%CI)以及AF或HF风险。潜在的混杂因素包括吸烟、早发冠心病家族史、体力活动、酒精摄入量、体重指数、干预组、血脂异常、高血压、2型糖尿病和药物使用情况。
研究人员比较了代谢物的四分位数,琥珀酸、苹果酸、柠檬酸和D/L-2-羟基戊二酸水平升高与较高的AF风险相关[Q4与Q1相比OR(95%CI):1.80(1.21-2.67)、2.13(1.45-3.13)、1.87(1.25-2.81)和1.95(1.31-2.90)]。附子酸增加1个SD与AF风险增加直接相关[OR(95%CI):1.16(1.01-1.34)]。苹果酸、乌头酸、异柠檬酸和D/L-2-羟基戊二酸Q4与Q1的四分位数相比,HF的相应OR(95%CI)分别为2.15(1.29-3.56)、2.16(1.25-3.72)、2.63(1.56-4.44)和1.82(1.10-3.04)。这些关联在内部验证中得到了确认,但附子酸和AF除外。
由此可见,这些结果突出了TCA循环在心脏结局发病机制中的潜在作用。
原始出处:
Mònica Bulló.et al.Tricarboxylic acid cycle related-metabolites and risk of atrial fibrillation and heart failure.Metabolism-Clinical and Experimental.2021.https://doi.org/10.1016/j.metabol.2021.154915
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险的关系#
45
#MET#
50
#Meta#
38
#代谢物#
36
#心衰风险#
44
#Metabolism#
51
#ABO#
42