Heart:妊娠相关的心血管疾病与患者结局的关系
2022-04-17 MedSci原创 MedSci原创
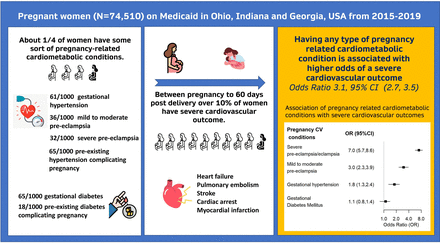
妇女在妊娠期间有较高的严重心血管疾病发生率。妊娠期间的心脏代谢状况使严重心血管疾病发生几率增加三倍。
在美国,每年大约有700名妇女死于与妊娠相关的并发症,其中超过33%的与妊娠相关的死亡是由心血管疾病造成的。尽管制定了降低孕产妇死亡率的目标,但令人担忧的是,美国的孕产妇死亡率上升了26.6%,从2000年的18.8人/10万活产上升到2014年的23.8人/10万活产。妊娠相关的心脏代谢疾病可能导致更严重的心血管疾病。
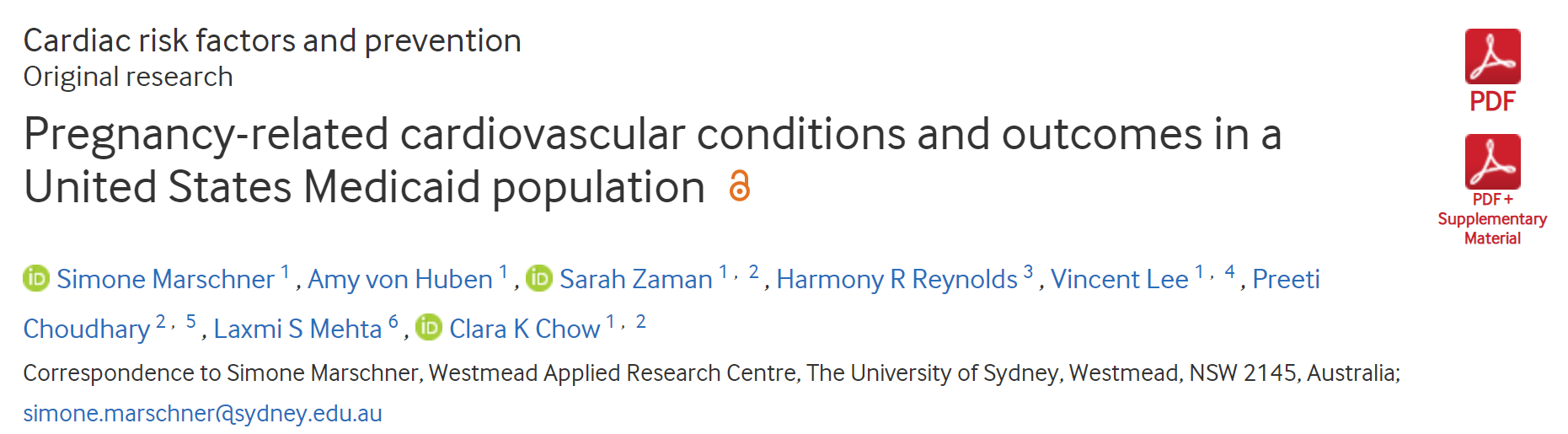
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究旨在调查美国医疗补助计划资助的女性与妊娠相关的心脏代谢疾病和严重心血管疾病的发生率,以及它们之间的关系。
医疗补助是美国政府资助的一项针对低收入家庭的医疗保险计划。研究人员报告了与妊娠相关的心脏代谢疾病(妊娠或妊娠合并的高血压疾病和糖尿病)和严重心血管疾病(心肌梗死、卒中、急性心力衰竭、心肌病、心脏骤停、心室颤动、心室心动过速、主动脉夹层/动脉瘤和外周血管疾病)。受试者为2015年1月至2019年6月期间来自乔治亚州、俄亥俄州和印第安纳州的医疗补助计划资助的生育(第十版国际疾病分类临床代码(ICD-10-CM)诊断代码为O80或O82)妇女。在这一横断面队列研究中,研究人员使用多变量模型评估了从妊娠到出生后60天期间妊娠相关的心脏代谢状况与严重心血管结局之间的关系。
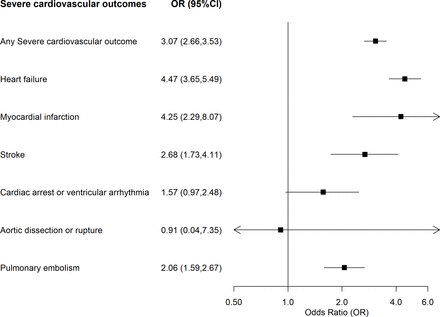
在74510名平均年龄为26.4岁(SD为5.5)的女性中,每1000名新生儿中妊娠相关心脏代谢疾病的发生率为224.3 (95%CI为221.3-227.3)。严重心血管疾病的发病率为10.8/1000 (95%CI为10.1至11.6)。与妊娠相关的心脏代谢疾病的女性患严重心血管疾病的风险更大,年龄调整OR为3.1(95%CI为2.7至3.5)。
由此可见,妇女在妊娠期间有较高的严重心血管疾病发生率。妊娠期间的心脏代谢状况使严重心血管疾病发生几率增加三倍。
原始出处:
Simone Marschner.et al.Pregnancy-related cardiovascular conditions and outcomes in a United States Medicaid population.heart.2022.https://heart.bmj.com/content/early/2022/04/13/heartjnl-2021-320684
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ART#
27
#患者结局#
27
#血管疾病#
29
#HEART#
28