ASH 2015:癌症相关血栓形成患者使用LMWH治疗6月后,可换为华法林治疗
2015-12-16 Mechront 译 MedSci原创
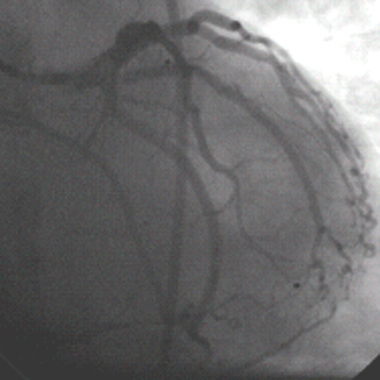
癌症相关血栓形成患者使用低分子肝素(LMWH)抗凝治疗6月后换成华法林继续抗凝治疗是安全的,并不会导致增加静脉血栓形成复发风险,也不会提高出血风险。建议癌症相关血栓形成患者一经诊断需使用LMWH抗凝治疗至少3-6个月,但是6个月之后抗凝治疗选用药物以及疗效并不明确。LMWH必需注射,而华法林可以口服。因此有研究者对这两种药物进行了比较。该研究纳入了1502名已经LMWH抗凝治疗6个月的患者,其中7
2015年第57届美国血液病学会(ASH)指出:癌症相关血栓形成患者使用低分子肝素(LMWH)抗凝治疗6月后换成华法林继续抗凝治疗是安全的,并不会导致增加静脉血栓形成复发风险,也不会提高出血风险。
建议癌症相关血栓形成患者一经诊断需使用LMWH抗凝治疗至少3-6个月,但是6个月之后抗凝治疗选用药物以及疗效并不明确。LMWH必需注射,而华法林可以口服。因此有研究者对这两种药物进行了比较。
该研究纳入了1502名已经LMWH抗凝治疗6个月的患者,其中763名患者继续LMWH治疗,还有739名患者则开始口服华法林治疗。以静脉血栓复发或肺栓塞作为初始结局指标;而出血(血红蛋白<20g/L或输红细胞悬液2U)关键器官出血、致命性出血等是继发结局指标。研究数据表明,两组静脉血栓复发率之间无差异(HR 0.67; P = .06),主要出血累计发生率LMWH组为2.6%,华法林组为2.7%(HR, 1.05; P = .79),总出血发生率LMWH组为6.7%,华法林组为7.0%(HR, 0.92: P = .70)。
随着医疗的发展,许多癌症已经不是死神般恐怖,反而越来越像慢性疾病,癌症患者寿命越来越长,一些与癌症相关血栓形成的患者则需要更长时间的抗凝治疗,LMWH不仅操作不方便,并且价格昂贵。而该研究表明,使用LMWH治疗6个月后,换为口服华法林并不会加重或延误病情,对该类患者这无疑是福音。
原始出处:
American Society of Hematology (ASH) 57th Annual Meeting. Abstract 430. Presented December 7, 2015.
Switch From LMWH to Warfarin OK in Cancer-Related Thrombosis
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#癌症相关血栓形成#
48
#癌症相关血栓#
28
赞
69
好文章,值得看。
97
学习了!赞!
45
#癌症相关#
32
#ASH#
28