BMC Med:高促甲状腺激素导致脂质谱异常和较高的心血管疾病风险
2021-12-20 从医路漫漫 MedSci原创
甲状腺功能减退和亚临床甲状腺功能减退与较高的总胆固醇、低密度脂蛋白胆固醇(LDL-c)和甘油三酯水平相关,亚临床甲状腺功能减退与较高的冠状动脉疾病(CAD)风险相关。
背景:甲状腺功能减退(定义为高促甲状腺激素(TSH)和低游离甲状腺素(FT4)水平)和亚临床甲状腺功能减退(定义为超出参考范围内的高TSH和FT4)与较高的总胆固醇、低密度脂蛋白胆固醇(LDL-c)和甘油三酯水平相关,亚临床甲状腺功能减退与较高的冠状动脉疾病(CAD)风险相关。然而,最近两项关于左甲状腺素治疗患有亚临床甲状腺功能减退症的老年人的随机安慰剂对照试验没有发现心血管事件的减少,这可能是由于缺乏统计能力所致。孟德尔随机化(MR)研究和使用代谢组学数据的研究可以进一步阐明甲状腺状况在冠心病中可能的因果作用。先前关于甲状腺状况和冠心病的MR研究是在多血统人群中进行的,而甲状腺功能、甲状腺功能障碍患病率和心肌梗死风险都因血统不同而不同。此外,仅在欧洲血统的人群中发现了甲状腺参数的遗传变异。我们假设,仅在欧洲样本中进行磁共振检查可以提供更准确的效果估计。此外,代谢组谱可以作为中间表型,用于研究疾病的早期亚临床阶段,特别是考虑到脂蛋白亚类及其含量时。最近,巴西一群人的研究结果显示,利用代谢组学平台,已经有希望的结果表明,亚临床甲状腺功能与不良的脂质状况有关。本研究旨在探讨甲状腺状态与心血管疾病之间的潜在因果关系,并描述与甲状腺状态相关的代谢谱特征。
方法:我们努力纳入尽可能多的队列,在欧洲血统的参与者中测量暴露和结果的数据。最后,来自6个欧洲血统队列的数据被用于循环代谢标志物浓度和甲状腺状况的第一阶段分析;500功能基因组研究(500FG)(n=421),遗传学、关节和进展研究(GARP)(n=321),莱顿长寿研究(LLS)(n=486),荷兰抑郁和焦虑研究(NESDA)(n=2906)[25],Prosper(n=5316)和鹿特丹研究(RS)(n=1690)。我们使用来自波美拉尼亚健康研究(SHIP)的数据作为验证(n=983),使用不同的代谢组学方法。每项参与的研究都获得了所有参与者的书面知情同意,并获得了适当的当地机构审查委员会的批准。通过多队列双样本孟德尔随机化(MR),利用全基因组显著性变异作为参考范围内标准促甲状腺素(TSH)和游离甲状腺素(fT4)的工具。TSH和fT4与代谢谱之间的关系通过两阶段的方式进行研究:首先评估TSH和fT4与全部161个代谢组标志物之间的相关性,然后通过孟德尔随机化(孟德尔随机化是另一种代谢谱平台)评估定向一致性,并在生物化学定义的甲状腺功能障碍的个体中。
结果:在9432名甲状腺正常个体(中位年龄从23.0岁到75.4岁不等,54.5%为女性)中,循环TSH与52/161代谢组标志物相关,FT4水平与21/ 161代谢组标志物相关。在多变量回归、MR、代谢组学平台以及甲亢患者中,循环TSH水平与极低密度脂蛋白亚类和组分、甘油三酯浓度和脂蛋白甘油三酯含量之间的正相关在方向上是一致的。FT4水平与TSH水平相反。91810 CAD病例和656091控制的欧洲血统,每1-SD增加的由基因决定的TSH浓度CAD的风险略有增加,但不显著,OR为1.03 (95% CI 0.99 - -1.07; P值=0.16 ),而较高的基因决定FT4水平不相关CAD风险(或1.00 / SD fT4增加;95% CI 0.96-1.04;p值=0.59)。
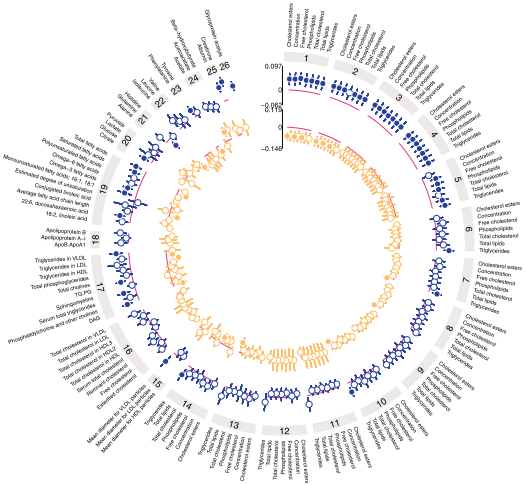
图1 参考范围内标准化TSH和FT4与161个南丁格尔平台代谢标志物之间的第一阶段相关性(N=9353)。点估计值代表代谢标记物浓度的标准化变化,根据TSH的标准偏差变化,根据年龄、性别、体重指数和吸烟进行调整。红条表示正值;蓝条表示负值。经多次检验校正后,空洞效应估计值无统计学意义(p值<1.34×10^3)。(1)极大极低密度脂蛋白(VLDL)。(2)极大极低密度脂蛋白(VLDL)。(3)大型极低密度脂蛋白(VLDL)。(4)中度极低密度脂蛋白(VLDL)。(5)小的极低密度脂蛋白(VLDL)。(6)极小的极低密度脂蛋白(VLDL)。(7)IDL。(8)大低密度脂蛋白(LDL)。(9)中度低密度脂蛋白(LDL)。(10)小低密度脂蛋白(LDL)。(11)非常大的高密度脂蛋白。(12)大高密度脂蛋白。(13)中等高密度脂蛋白(HDL)。(14)小高密度脂蛋白(HDL)。(15)脂蛋白颗粒大小。(16)胆固醇。(17)甘油酯和磷脂。(18)载脂蛋白。(19)脂肪酸。(20)糖酵解相关代谢物。(21)氨基酸。(22)支链氨基酸。(23)芳香氨基酸。(24)酮体。(25)液体平衡。(26)炎症。HDL,高密度脂蛋白;LDL,低密度脂蛋白;VLDL,极低密度脂蛋白
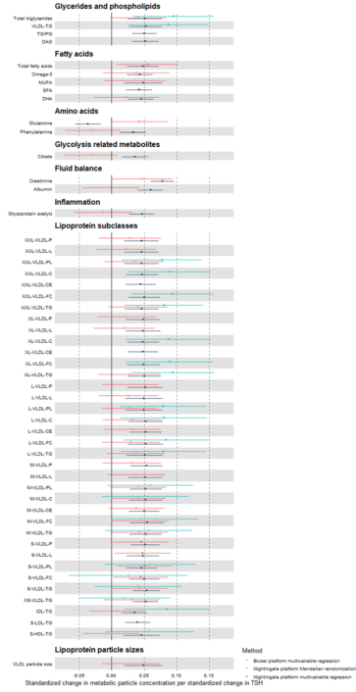
图2 在Nightingale平台上使用多变量和孟德尔随机化分析,在Bruker平台上使用多变量分析,TSH与52个代谢组标志物之间的第二阶段关联。点估计代表TSH每标准差变化的代谢组学标记物浓度的标准化变化;误差条表示95%置信区间。多变量分析根据年龄、性别、体重指数和吸烟情况进行调整,孟德尔随机化分析采用逆方差加权(IVW)估计。空心效应估计指的是与p值 > 0.05的关联

图3 参考范围内基因决定的标准化TSH和FT4与冠状动脉疾病之间的相关性(91,810例CAD病例和656,091例欧洲血统对照)。比值比(or)显示(每1 s.d.增加TSH/FT4浓度)是逆方差加权(IVW)估计,MR Egger和加权中位数估计;误差条表示95%置信区间
结论:甲减导致血脂水平异常和某种程度上增加心血管疾病的风险。
原文出处:
van Vliet NA, Bos MM, Thesing CS,et al.Higher thyrotropin leads to unfavorable lipid profile and somewhat higher cardiovascular disease risk: evidence from multi-cohort Mendelian randomization and metabolomic profiling.BMC Med 2021 Nov 03;19(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMC#
47
点赞
56
#促甲状腺激素#
50
#疾病风险#
46
#血管疾病#
50
#质谱#
45
#Med#
32