NAT IMMUNOL:重磅!癌症治疗新突破,癌细胞发现第二个“不吃我”的信号
2017-11-28 MedSci MedSci原创
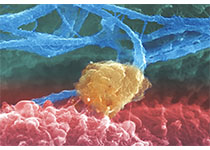
斯坦福大学医学院(Stanford University School of Medicine)的研究人员发现了另一种生物途径,即信号免疫细胞不会吞噬和杀死癌细胞。
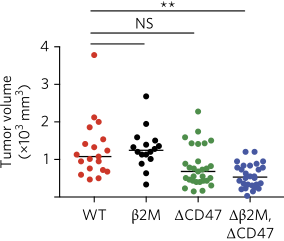
MHCI+CD47+(WT)、MHCI-CD47+(β2M)
MHCI+CD47-(ΔCD47)、MHCI-CD47-(Δβ2M,CD47)
阻断“不吃我”信号的抗体已经在动物模型中显示出作为癌症治疗的希望,目前正在进行临床试验。研究人员认为,将这种称为抗CD47的抗体与另一种阻断这种新发现的通路的抗体结合,可以进一步提高免疫系统根除多种类型癌症的能力。
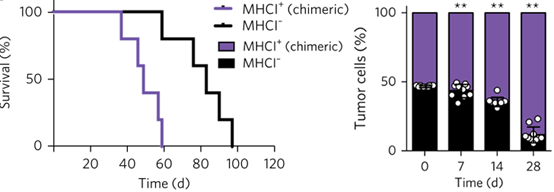
在体内,癌细胞表达的1类MHC保护其免受巨噬细胞攻击
斯坦福大学干细胞生物学和再生医学研究所所长欧文·韦斯曼(Irving Weissman),也是路德维希癌症中心的主任说。“癌细胞的发展触发了人体清道夫细胞识别的SOS分子的产生,称为巨噬细胞。 “然而,侵略性的癌症表面上以CD47的形式表达了”不吃我“的信号,现在我们已经发现了第二个”不吃我“的信号及其在巨噬细胞上的互补受体。表明我们可以用特定的抗体克服这个信号,恢复巨噬细胞杀死癌细胞的能力。
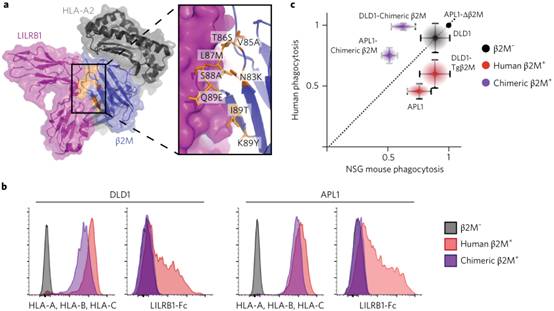
巨噬细胞表面的LILRB1与癌细胞上1类MHC结构的β2M结合(图片来源 Nature)
描述这些发现的论文在11月27日在Nature Immunology上发表。
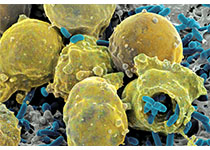
Barkal说:同时阻断这两种小鼠的这些途径导致了肿瘤与许多类型的免疫细胞的潜入,并且显着促进了肿瘤清除,导致整体上变小的肿瘤。 我们对能够在人体内进行双重或甚至三重治疗的可能性感到兴奋,因为我们将多重阻滞与癌症发展相结合。
巨噬细胞的重要性
巨噬细胞是在几乎所有身体组织中发现的大量白血细胞。 作为先天免疫系统的组成部分,它们吞噬和杀死细菌或病毒等外来侵略者。 它们还会摧毁死亡和死亡的细胞,在某些情况下还会破坏其内部发育线索已经失效的癌细胞。
2009年,韦斯曼实验室发现了“不吃我”的信号。他的研究小组发现,几乎所有的癌细胞表面都有高水平的CD47分子。他们发现,CD47在巨噬细胞表面与一种名为SIRPalpha的蛋白质结合,抑制了它们杀死癌细胞的能力。
动物研究表明,抗cd47抗体的治疗大大提高了巨噬细胞杀死癌细胞的能力,甚至导致了小鼠癌症模型的某些治疗。第一阶段临床试验目前正在斯坦福大学和联合王国进行,以测试各种血液和实体肿瘤的治疗对人类的安全性和有效性。
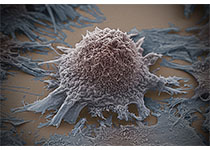
新发现的用于癌症细胞逃避巨噬细胞的具有约束力的相互作用,利用癌细胞表面的一种蛋白质结构,称为主要组织相容性复合体1,或MHC类1。研究人员发现,在他们的表面有高水平MHC等级1的人肿瘤对抗cd47治疗的抵抗力比那些低水平的人肿瘤更强。
适应性免疫成分
MHC 1类是适应性免疫的重要组成部分,它是免疫系统的第二主要组成部分,依赖免疫细胞称为T细胞和B细胞,灵活而特异地应对外来入侵者和细胞损伤。身体的大多数细胞在其表面上表达MHC类别1,以便无差别地显示细胞内发现的许多蛋白质的位点 - 一种细胞内脏的随机取样,为其健康和功能提供了一个窗口。如果由MHC显示的称为肽的蛋白质位异常,则T细胞破坏细胞。虽然MHC 1类和T细胞之间的关系已经确立,但是复合物是否以及如何与巨噬细胞相互作用尚不清楚。
巴卡尔和她的同事们发现,巨噬细胞表面的一种名为LILRB1的蛋白质与人类广泛分享的肿瘤细胞上MHC1类的一部分结合。研究人员发现,这种结合抑制巨噬细胞吞噬和杀死癌细胞的能力,无论是在实验室培养皿中还是在具有人类肿瘤的小鼠中生长。抑制CD47介导的途径和LILRB1途径显着减缓小鼠中的肿瘤生长。
了解适应性和先天性免疫之间的平衡在癌症免疫治疗中是重要的。例如,人类癌细胞在其表面上降低MHC类别1的水平以避免T细胞破坏并不罕见。患有这些类型的肿瘤的人可能是用于癌症免疫疗法的不良候选者,所述癌症免疫疗法旨在刺激针对癌症的T细胞活性。但研究人员认为,这些细胞可能特别容易受到抗CD47的治疗。相反,在其表面上具有强的MHC类别1的癌细胞可能不易受抗CD47的影响。
Weissman说:“在某些癌症中,由于多种原因,MHC1类的表达并没有减少,这有助于癌细胞从巨噬细胞中逃脱出来,这些发现帮助我们了解癌细胞能够逃避巨噬细胞的多种方式,我们如何阻止这些逃生途径。
Barkal说:“至少有两种调节巨噬细胞活性的多余机制,证明了严格控制我们的免疫反应是至关重要的。 “未来的研究有可能确定更多这些途径,这将为我们提供癌症免疫治疗的额外目标。”
Amira A. Barkal, Kipp Weiskopf, Kevin S. Kao, et al.Engagement of MHC class I by the inhibitory receptor LILRB1 suppresses macrophages and is a target of cancer immunotherapy.Nature Immunology (2017) doi:10.1038/s41590-017-0004-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#癌症治疗#
35
#新突破#
27
#Nat#
33
值得进一步研究
53
值得进一步研究
62
#癌细胞#
20
#重磅#
22
不错的.学习了!谢谢分享!
43
学习了新知识
45
学习了.涨知识
51