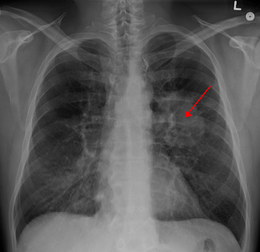
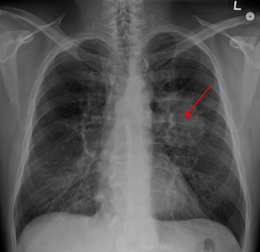
CLIN CANCER RES:RCC2过表达促进肺腺癌转移
2017-09-24 MedSci MedSci原创
CLIN CANCER RES近期发表了一篇文章,研究RCC2在肺腺癌转移中扮演的角色。
CLIN CANCER RES近期发表了一篇文章,研究RCC2在肺腺癌转移中扮演的角色。作者使用临床肿瘤标本评估RCC2对肺腺癌转移的影响。使用鼠模型、细胞生物学、分子生物学等手段阐明RCC2在肺腺癌中的功能及其作用机制。研究结果表明,在肺腺癌中RCC2表达普遍上调(88/122,72.13%)。通过分析包含了488例肺腺癌和58例正常肺组织的TCGA RNA-seq数据进一步验证了这一结果。RCC2水平升高与肿瘤T分期,淋巴结转移和晚期临床分期显着相关。RCC2表达水平更高的肺腺癌患者总生存期更短。Cox回归分析结果表明RCC2是肺腺癌患者不良预后的独立预测因素。此外,体内实验中人为增加RCC2表达可以促进肿瘤肺内转移,在体外实验中则可以显着促进肺腺癌细胞迁移、侵袭和增殖。进一步研究表明RCC2可以诱导上皮细胞间质转化(EMT),并可以刺激MMP-2和MMP-9表达。此外,RCC2可以激活JNK,阻断JNK可以抑制RCC2对肺腺癌细胞迁移、侵袭、EMT和MMP-2、MMP-9的影响。文章最后认为,RCC2通过激活MAPK-JNK信号通路诱导上皮细胞间质化在肺腺癌转移中起到了重要的作用
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#RCC#
33
#过表达#
31
#癌转移#
0
学习了.谢谢分享
54
学习了受益匪浅
56
好文章.学习了.
47