JCEM:多模式治疗或能改善甲状腺未分化癌的预后
2017-10-31 MedSci MedSci原创
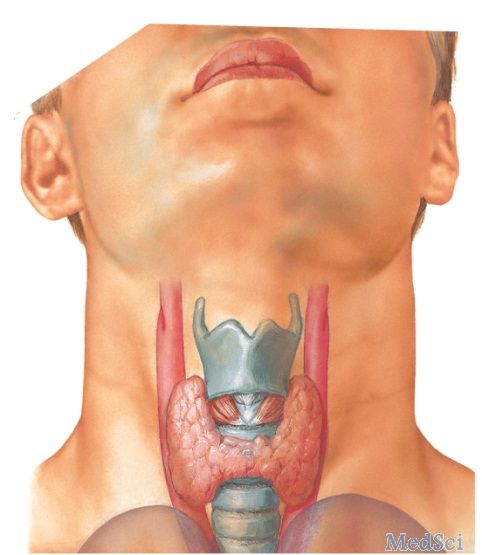
背景:甲状腺未分化癌(anaplastic thyroid cancer,ATC)是甲状腺癌中恶性程度最高的一种,发病率约占全部甲状腺癌的10-15%,多见了年老体弱者,发病迅速, 早期可发生全身转移,一般认为多发生白良性肿瘤或低恶性肿瘤。ATC恶性程度高,预后差,其历史结局令人沮丧。目的:本研究旨在确定最初的结合手术、化疗和放疗的多模式强化治疗是否能改善ATC生存率。方法:2003-2015年间
背景:甲状腺未分化癌(anaplastic thyroid cancer,ATC)是甲状腺癌中恶性程度最高的一种,发病率约占全部甲状腺癌的10-15%,多见了年老体弱者,发病迅速, 早期可发生全身转移,一般认为多发生白良性肿瘤或低恶性肿瘤。ATC恶性程度高,预后差,其历史结局令人沮丧。目的:本研究旨在确定最初的结合手术、化疗和放疗的多模式强化治疗是否能改善ATC生存率。方法:2003-2015年间,在梅奥诊所接受多模式治疗的所有新诊断ATC患者被纳入了本研究;考虑临床状态和患者偏好个性化给予多模式治疗 vs 姑息治疗。研究人员采用AJCC分期对结果进行回顾性分析,并将结果与机构审查委员会批准的1949-1999患者队列数据进行对比。研究共纳入了48例患者,其中18例接受姑息治疗,30例接受多模式治疗(60%为男性,中位年龄为62岁)。AJCC分期IVA、IVB和IVC ATC分别为2例、27例和18例;随访中位数为20个月。主要结果测量:使用Kaplan Meier法统计的总体无进展生存率(ATC诊断的OS、PFS)。结果:2003-2015年队列的中位总生存期为9个月(95% CI,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCE#
0
#分化癌#
45
#甲状腺未分化癌#
41
#JCEM#
35
内容很好.收藏了.以后用的到
49
学习了.谢谢
42