重度抑郁症新药Zuranolone,疗效迅速且明显
2022-02-19 Allan MedSci原创
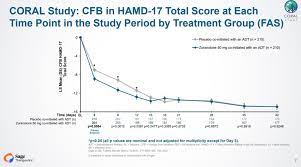
研究 zuranolone 治疗重度抑郁症(MDD)的 III 期 CORAL 研究达到了主要和关键次要终点,表明在第三天和两周内抑郁症状“迅速且具有统计学意义的减少”。
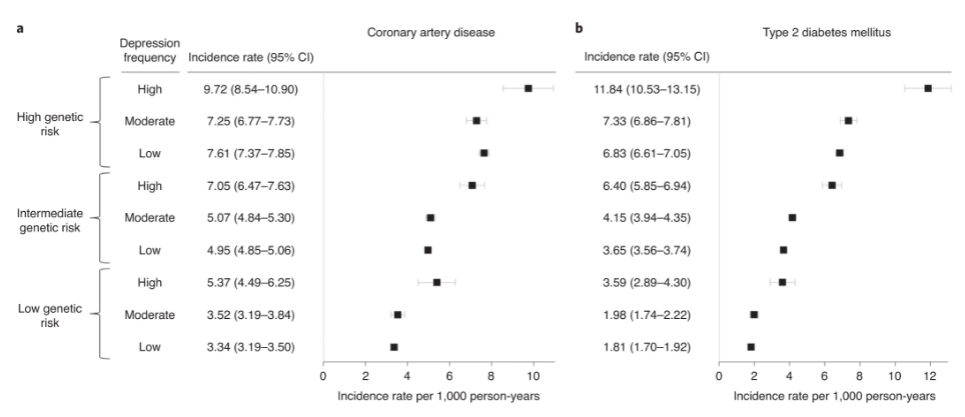
抑郁症是一种心境障碍,会令人持续感觉忧伤和丧失兴趣。抑郁症也称为重度抑郁障碍或临床抑郁症,会影响患者的感受、思维和行为,可能导致各种情绪和身体问题。
Biogen 和 Sage Therapeutics 本周三表示,研究 zuranolone 治疗重度抑郁症(MDD)的 III 期 CORAL 研究达到了主要和关键次要终点,表明在第三天和两周内抑郁症状“迅速且具有统计学意义的减少”。
CORAL 招募了 440 例患有 MDD 的成年人,他们在 17 项汉密尔顿抑郁量表 (HAMD-17) 上的平均基线得分为 26.6-26.8。参与者被随机分配接受 zuranolone 或安慰剂(均接受标准护理治疗),每晚一次,持续两周。对于主要终点,结果显示 zuranolone 导致 HAMD-17 总分从基线变化为 -8.9,而安慰剂组为 -7。Zuranolone 还达到了关键次要终点,表明在两周的治疗期内抑郁症状得到了显著改善。在此期间,患者在 HAMD-17 量表上的平均变化为 -11.7 分(zuranolone 组),而安慰剂组为 -10.1。
关于安全性,两家公司表示,大多数 CORAL 试验的受试者经历了轻中度治疗相关不良事件 (TEAE)。 zuranolone组患者因 TEAE 导致的停药率为 6.6%,安慰剂组为 3.7%。zuranolone 组患者最常见的 AE 是嗜睡,影响了 18.4% 的患者。制药商指出,没有证据表明服用该药物的患者自杀意念或行为的增加。
Zuranolone 是 GABAA 受体的新一代正向变构调节剂,目前正处于 MDD 和产后抑郁症 (PPD) 的后期开发阶段。去年,Biogen 和 Sage Therapeutics 宣布计划在 2022 年下半年开始向 FDA 滚动提交关于 zuranolone 用于 MDD 的申请,并计划在 2023 年上半年提交关于 zuranolone 用于 PPD 的申请。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习
55
了解了解
60
#抑郁#
93
学习
60