椎管内肿瘤切除术
2016-03-14 MedSci www.windrug.com
椎管内肿瘤切除术 椎管内肿瘤见于脊髓的任何节段和马尾神经,以胸段最常见。可发生于任何年龄,但以20~40岁之间的成年人占多数。按解剖部位分硬脊膜外、髓外硬脊膜内。髓内3大类。按病理分类以神经纤维瘤、脊膜瘤及胶质细胞瘤(包括星形细胞瘤及室管膜瘤)3种最为常见。椎管内肿瘤中良性者居多,唯一有效的治疗方法是手术切除肿瘤,约3/4可手术切除治愈。病人年龄即使较大,如70岁以上,有时亦可较好地耐受手术。因
椎管内肿瘤切除术
椎管内肿瘤见于脊髓的任何节段和马尾神经,以胸段最常见。可发生于任何年龄,但以20~40岁之间的成年人占多数。按解剖部位分硬脊膜外、髓外硬脊膜内。髓内3大类。按病理分类以神经纤维瘤、脊膜瘤及胶质细胞瘤(包括星形细胞瘤及室管膜瘤)3种最为常见。椎管内肿瘤中良性者居多,唯一有效的治疗方法是手术切除肿瘤,约3/4可手术切除治愈。病人年龄即使较大,如70岁以上,有时亦可较好地耐受手术。因此,对椎管内肿瘤的手术应持积极态度,除病人情况确定不能耐受手术者外,一旦确诊为椎管内肿瘤,不论脊髓受压程度的轻重,均应及时手术治疗。
[适应证]
有脊髓压迫症状及体征,经腰椎穿刺、X线摄片等一般检查及脊髓造影、CT扫描、磁共振成像或脊髓血管造影等特殊检查,证实为椎管内占位性病变压迫脊髓者。
[术前准备]
同椎管-脊髓探查术。
[麻醉]
全麻或硬脊膜外麻醉。
一、硬脊膜外肿瘤切除术
硬脊膜外肿瘤可占椎管内肿瘤的17%~25%,良性肿瘤如脊膜瘤、神经纤维瘤、骨瘤、软骨瘤、血管瘤、脊索瘤等较少见,恶性肿瘤中转移性多于原发性,转移性癌的原发灶以肺癌及淋巴肉瘤最多见,其次在肝癌、消化道癌肿等。
硬脊膜外良性肿瘤压迫脊髓者均应手术治疗。恶性肿瘤由于根治困难,一旦临床表现有神经根和脊髓明显受损征象,即使外科手术摘除肿瘤,也难以使受损的神经功能有所恢复。
因此一般只对可能切除的单发病灶,以及病人情况佳,为了减压或活组织检查以明确诊断作为综合治疗的依据时方考虑手术。反之,如病人身体衰竭或伴有严重并发症(如肺炎、褥疮等),或完全截瘫3个月以上,或原发癌已广泛转移者,都不宜手术治疗。
[手术步骤]
 |
| 1-1 椎板切除,显露肿瘤 |
1.切口及椎板减压 侧卧位或俯卧位。以肿瘤的中央为中心设计切口,其手术操作步骤与椎管-脊髓探查术相仿。按脊髓造影或临床定位切除椎板后即见肿瘤,上下扩大手术野至肿瘤上下端增色已显露为止[图1-1]。
 |
| 1-2 切除硬脊膜外肿瘤的背侧部分 |
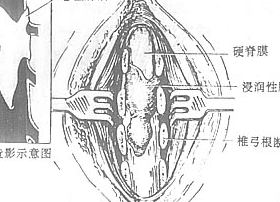
2.切除肿瘤 肿瘤显露后如系良性肿瘤,从肿瘤上极或下极开始剥离。如系硬脊膜瘤,肿瘤附着的硬膜应一并切除,缺损处用筋膜修复。如系神经纤维瘤,附着的神经根如确定不能保留者始予切断。如突向椎间孔,应探查是否突向椎间孔外成为哑铃形肿瘤,其切除方法同图9-6,7。恶性肿瘤与硬脊膜粘连大多广泛而紧密,切除时渗血多,完全切除多有困难,可大部切除以达减压目的。如有必要可取一块作冰冻切片检查。决定切除后,从肿瘤边缘开始,交替用剪刀、刮匙、活组织等沿硬脊膜把肿瘤切除[图1-2],渗血用双极电凝及明胶海绵压迫等止血。如肿瘤已蔓延至硬脊膜腹侧时,可轻轻推开硬脊膜,用活组织钳或刮匙尽量清除[图1-3]。转移癌大部切除后,加上椎板减压,术后可作放射治疗或化学治疗。骶棘肌作2~3层缝合,严密缝合皮下组织及皮肤,不放引流管,以免肿瘤沿引流管几外扩散[图1-4]。
 |
| 1-3 切除硬脊膜外肿瘤的腹侧部分 |
 |
| 1-4 缝合 |
| 图1 硬脊膜外肿瘤切除术 |
3.后根切断 如肿瘤压迫或浸润神经根引起剧痛,其它方法治疗无效时,可同时作受浸润的脊神经后根切断术。方法是在肿瘤切除后,在该处把硬脊膜沿中线切开,分离出受侵犯的脊神经后根,该神经根在两侧齿状韧带之后,易于[图2-1]。小心从后根处分离出脊神经血管以免损伤,这是避免术后脊髓缺血的重要措施。然后用止血钳压榨后切断[图2-2、3]。切断神经根的数目可视临床需要而定,但不宜过多。彻底止血后冲洗脊髓腔,间断缝合硬脊膜,其它各层缝合同前述。
 |
| 2-1 脊神经后根及其与血管的关系 |
 |
| 2-2 压榨后根 |
 |
| 2-3 切断后根 |
| 图2 脊神经后根切除术 |
[术中注意事项]
肿瘤切除后,硬脊膜膨起搏动良好,一般不必再切开硬脊膜探查。
[术后处理]
同椎管、脊髓探查术。如系恶性肿瘤,则应予拆线后开始放射治疗或化学治疗,并处理转移癌的原发灶。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#椎管内#
30
#椎管#
43
#肿瘤切除#
37
#切除术#
36
这篇文章值得收藏
82
好详细
111
内容很精彩
103