NEJM:戈舍瑞林可有效保护化疗期间乳癌患者的卵巢功能
2015-03-05 Mechront MedSci原创
随着检测技术的提高,乳腺癌患者不仅越来越多,还越来越年轻化。辅助化疗是乳腺癌治疗的常用手段,但其对卵巢有不可估量的毒副作用,常导致卵巢功能衰竭。在激素受体阴性的乳腺癌女性患者中,化疗过程中使用措施对卵巢进行保护是迫切需要的。目前学术界有关于GnRH激动剂保护卵巢功能的研究报道,但所得结果有好有坏,仍存争议,并且缺乏关于此类女性妊娠结局的数据。因此Halle C.F.等人在2004-02至
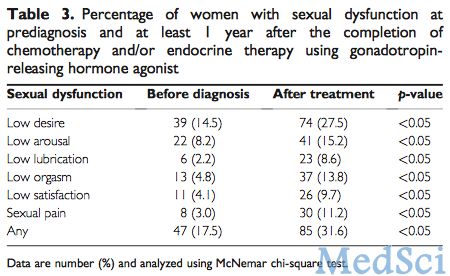
随着检测技术的提高,乳腺癌患者不仅越来越多,还越来越年轻化。辅助化疗是乳腺癌治疗的常用手段,但其对卵巢有不可估量的毒副作用,常导致卵巢功能衰竭。在激素受体阴性的乳腺癌女性患者中,化疗过程中使用措施对卵巢进行保护是迫切需要的。目前学术界有关于GnRH激动剂保护卵巢功能的研究报道,但所得结果有好有坏,仍存争议,并且缺乏关于此类女性妊娠结局的数据。因此Halle C.F.等人在2004-02至2011-05期间进行了一项研究以探究GnRH激动剂戈舍瑞林在化疗过程中对女性卵巢功能的保护作用。最新研究成果发表在近期NEJM上。
最终参与该研究的为218名未绝经女性,均为可手术、激素受体阴性的乳腺癌患者。研究者将其随机分为两组,试验组为化疗加GnRH激动剂戈舍瑞林(N=105),对照组只使用化疗(N=113)。以第2年卵巢功能衰竭作为原始结局指标,卵巢功能衰竭定义为:在这之前6个月都没有来月经,FSH水平处于绝经后范围。以妊娠结局、无病生存率和总生存率作为次级结局指标。
该研究结果显示,218名参与者中,有135名得到了原始结局指标,试验组卵巢功能衰竭数据为8%,对照组有22%,两组比较,OR=0.20,95% CI 0.09-0.97,P=0.04。因缺乏数据较多,对其进行敏感性分析之后,得出该结果是稳健的。缺乏数据在不同治疗组,或根据年龄、化疗等分层因素分层后没有差异。该研究还得出,在218名参与女性中,试验组和对照组妊娠数据为:21% vs. 11%,P=0.03。试验组无病生存率得到改善,P=0.004;试验组总生存率得到改善,P=0.05。
该研究结果表明,GnRH激动剂戈舍瑞林可以有效保护化疗期间乳腺癌患者的卵巢功能,避免卵巢功能衰竭,减少提前进入更年期的风险,改善其生育率。
原始出处:
Moore HC1, Unger JM, Phillips KA, Boyle F, Hitre E, Porter D, Francis PA, Goldstein LJ, Gomez HL, Vallejos CS, Partridge AH, Dakhil SR, Garcia AA, Gralow J, Lombard JM, Forbes JF, Martino S, Barlow WE, Fabian CJ, Minasian L, Meyskens FL Jr, Gelber RD, Hortobagyi GN, Albain KS; the POEMS/S0230 Investigators.Goserelin for Ovarian Protection during Breast-Cancer Adjuvant Chemotherapy.N Engl J Med. 2015 Mar 5;372(10):923-932.
本文是Medsci原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#戈舍瑞林#
37
很不错学习了
93
又进一步
142
#卵巢功能#
0
#卵巢功能#
39